Angina Pectoris
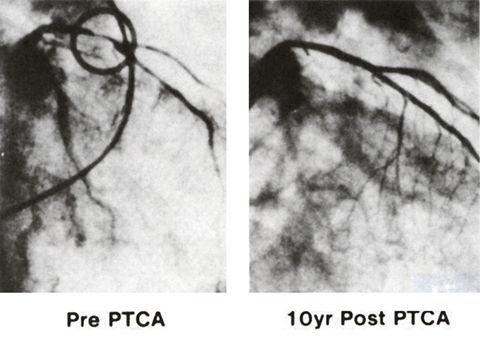
Figure 53
Right anterior oblique coronary arteriogram of the first patient who underwent the first transluminal coronary angioplasty on September 16, 1977 (left) by Andreas R. Gruentzig, M.D., and on September 16, 1987 (right). During this 10-year period, the patient remained completely asymptomatic and the arteriogram at 10 years showed no narrowing in the coronary arteries.
Douglas, Jr., J.S., M.D., King, III, S.B., M.D., Techniques of Percutaneous Transluminal Angiopasty and Atherectomy of the Coronary Arteries, The Hurst's The Heart, 8th ed., p 1346.
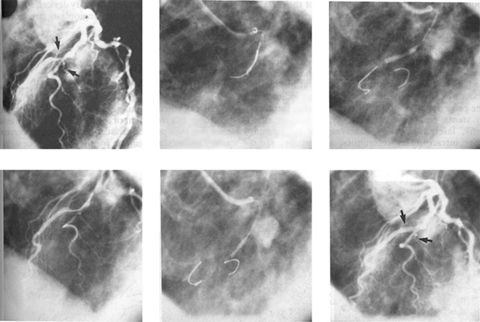
Figure 54
Angioplasty of high-grade stenosis of the left anterior descending artery diagonal bifurcation (see arrow) using a single guiding catheter through which two dilatation devices (USCI Probe) were passed. The left anterior descending artery was dilated with a 2.5-mm balloon, and the diagonal was dilated with a 2-mm balloon. Note small initmal tear in the left anterior descending artery following the small procedure (left anterior oblique views).
Douglas, Jr., J.S., M.D., King, III, S.B., M.D., Techniques of Percutaneous Transluminal Angiopasty and Atherectomy of the Coronary Arteries, The Hurst's The Heart, 8th ed., p 1347.
This term refers to midsternal, anterior chest pain due to a partially blocked coronary artery (see figures 53 and 54), often felt as a chest pressure like an elephant sitting on one's chest, spreading to the inner aspect of the upper left arm, neck and upper mid back, lasting anywhere from 5 to 10 or more minutes.
It is precipitated by excitement, exertion, or other stimuli that increase heart muscle oxygen requirements. The threshold for pain is usually fixed, but somewhat variable due to variations in the vasomotor tone and degree of vasospasm (see definition).
The blockage or occlusion of the coronary artery is due to atherosclerosis (see figure 70), which alters the ability of the coronary arteries to dilate. This contributes to the arteries being in vasospasm (see definition), which is abnormal. These arteries have enhanced vasospastic tone.
Recommended Drug Therapy (Calcium Antagonist versus Beta Blocker) in Patients with Angina associated Conditions(Gibbons et al.ACC/AHA/ACP ASIM Guidelines for the Management of Patients with Chronic stable Angina, J Mm.Coll. Cardiol. 1999:33:2097-2197.
Condition |
Recommended Treatment and Alternative |
Avoid |
|
Medical conditions Systemic hypertension Asthma or chronic obstructive pulmonary
disease with bronchospasm. Hyperthyroidism. Raynaud's syndrome. Insulin-dependent diabetes mellitus
Depression. Mild peripheral vascular disease Cardiac arrhythmias and conduction abnormalities. Sinus bradycardia. Sinus tachycardia (not due to heart
failure). Supraventncular tachycardia. Atrioventricular block. Rapid artrial fibrillation (with digitalis). Ventricular arrhythmias Left-sided valvular heart disease. Mitral regurgitation. Mitral stenosis |
Betablockers (calcium antagonists) Verapamil or Diltiazem Beta blockers. Long-acting slow-release calcium antagonists. Beta blockers (particularly if prior
myocardial infarction) or long-acting slow-release calcium
antagonists
Beta blockers or calcium antagonists Long-acting slow-release calcium antagonists
that do not decrease heart rate Verapamil, diltiazem, or beta blockers. Long-acting slow-release calcium antagonists
that do not slow AV conduction. Verapamil, diltiazem, or beta blockers. Beta blockers.
Beta blockers Long-acting slow-release dihydropyridines nondihydropyridine calcium antagonist |
Beta blockers Beta blockers Beta blockers. Beta blockers Beta blockers Beta blockers. Verapamil, diltiazem. Verapamil, diltiazem. Nitrates, dihydropyridine, calcium antagonists |
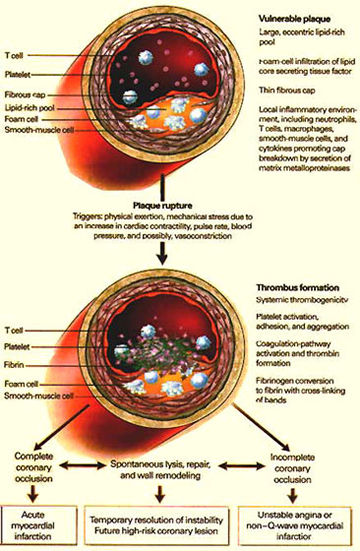
Figure 70
Pathophysiologic Events Culminating in the Clinical Syndrome of Unstable Angina. Numerous physiologic triggers probably initiate the rupture of a vulnerable plaque. Rupture leads to the activation, adhesion, and aggregation of platelets and the activation of the clotting cascade, resulting in the formation of an occlusive thrombus (clot). If this process leads to complete occlusion of the artery, then acute myocardial infarction with EKG ST-segment elevation (which indicates heart muscle injury) occurs. Alternatively, if the process leads to severe stenosis but the artery nonetheless remains patent, then unstable angina occurs.