Exercise testing elicits
the body's reaction to measured increases in acute exercise.The
changes in heart rate,blood pressure,respiration,and perceived
level of exercise provide data that permit quantitative estimation
of cardiovascular conditioning and function.Exercise tests provide
an opportunity to observe a personduring exercise.By monitoring
heart rate and blood pressure and continually observing the
ECG, one can detect changes in the hemodynamic response and
ischemic type ECG ST segment depression, and can detect and
classify disturbances in heart rhythm and conduction associated
with exercise.
THE CARDIOVASCULAR
RESPONSE TO EXERCISE
Exercise can elicit
cardiovascular abnormalities not present at rest and can be
used to assess function of the cardiovascular system. Isotonic
(dynamic) exercise, defined as muscular contraction of large
muscle groups resulting in movement, primarily provides a volume
load to the left ventricle, and thecardiovascular response is
proportional to the degree of the exercise.
Maximum Oxygen Uptake
When dynamic exercise
begins, oxygen uptake by the lungs quickly increases. After
several minutes,oxygen uptake usually remains relatively stable
(steady state) at each intensity of exercise.During the steady
state, the heart rate(HR), cardiac output,blood pressure, and
pulmonary ventilation are maintained at reasonably constant
levels.
Maximal oxygen consumption(Vo2max)
is the greatest amount of oxgen a person can utilize while performing
dynamic exercise involving large components of total muscle
mass and represents the amount of oxygen transported and used
in cellular metabolism.It is convenient to express oxygen uptake
in multiples of sitting/resting requirements.The metabolic equivalent(MET)
is a unit of sitting/resting oxygen uptake (3.5ml O2 per kilogram
of body weight per minute(ml kg-1min-1).Rather than determining
each person's true resting oxygen uptake,one MET is designated
as this average.resting oxygen uptake.Vo2max is significantly
related to age,gender,exercise habits,heredity, and clinicalcardiovascular
status
Maximum Vo2 is equal
to maximum cardiac output times maximum arteriovenous oxygen(aVo2)
difference.Since cardiac output is equal to the product of stroke
volume and heart rate(HR),Vo2 is directly related to HR.The
maximum aVo2 difference during exercise has a physiological
limit of 15 to 17 ml/dl;therefore,if maximum effort is achieved,Vo2max
can be used to estimate maximum cardiac output.
Myocardial OxygenUptake
Myocardial oxygen
uptake(Mo2) is determined by intramyocardial wall tension (left
ventricular(LV) systolic pressure times end-diastolic volume,
divided by LV wall thickness), contractility, and HR.Mo2 can
be estimated during exercise testing by the product of HR and
systolic blood pressure, called rate pressure product.
In general there is
a linear relation between Mo2 and coronary blood flow. During
exercise,coronary blood flow increases as much as five fold
above the resting value. A patient with obstructive coronary
disease,however,may not have enough coronary blood flow to supply
the metabolic demands of the myocardium during vigorous exercise,
and as a consequence,myocardial ischemia occurs.
RESPONSE TO DYNAMIC EXERCISE
The response to dynamic
exercise consists of a complex series of cardiovascular adjustments
to provide active musclec with blood appropriate for metabolic
needs,to dissipate heat generated by by active, and to maintain
blood supply toessential organs such as thebrain and heart.
As cardiac output
increases with dynamic exercise,vasculr resistance decreases
in active muscles but increases in tissues that do not function
during exercise. Since flow to active muscles increases much
more than arterial pressure, there is a significant decrease
invascular resistance.
Heart Rate Response
An increase in HR
due to a decrease in vagal outflow is an immediate response
of the cardiovascular system to exerciseThis is rapidly followed
by an increase in sympathetic outflow to the heart and systemic
blood vessels, which contribute to the increase in HR
Arterial Blood Pressure Response
Systolic blood pressure
increase with dynamic work as a result of increasing cardiac
output,while diastlic pressure usually remains about the same
or decreases slightly. Paients who develop hypotension during
exercise frequently have severe heart disease; patients with
aortic valvular disease can also exhibit a drop in systolic
pressure.
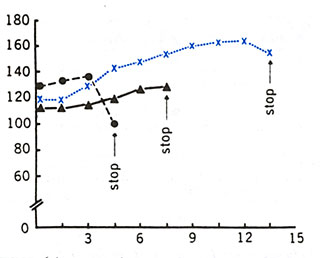
After maximal exercise,
there is normally a decrease in systolic blood pressure,usually
reaching resting levels in 6 mins., then often remaining lower
than pre-exercise for several hours.In some patients with coronary
artery disease(CAD), higher levels of systolic blood pressure,
at times even exceeding peak exercise values,may develop in
the recovery phase (Figure181). When exercise is terminated
abruptly, some healthy persons have precipitous drops in systolic
blood pressure due to venous pooling. Figure 181 shows the physiologic
response to submaximum and maximum treadmill exercise based
on tests of more than 700 apparently healhy men aged 25 t0 54.Maximalrate-pressure
product ranges from a 10th percentile value of 25,000 to a 90th
percentile of 40,000.
The arterial blood
supply to the myocardium and to the other muscles and organs
is usually adequate for the maximal perfusion requirement of
which the organ is capable. If obstructive disease is present
within a coronary artery, only minimal reduction in maximal
blood flow will take place until the degree of arterial obstrution
becomes quite advanced.The predictive importance of exertional
myocardial ischemia is related to the intensity of cardiac activity
at which the ischemia became apparent. For example,if there
is no evidence of ischemia at 75% of maximum exercise, but there
is at 90-100% of maximal exercise, it would likely be associated
with a less severe degree of coronary obstruction than if the
ischemia had been detectable at only 25-50% of maximal exercise.
Reference:Fletcher,G.F.,and Schlant,R.C.,The
Exercise Test,Hurst's The Heart,8th Edition,Pp.423-440.
TESTING PROCEDURES
Exercise testing of
patients should be conducted only by well-trained personnel
with a basic knowledge of exercise physiology. In general, only
physicians and other health professionals(especially nurses)
familiar with normal and abnormal responses during exercise
and qualified in Advanced Cardiac Life Support have the cognitive
skills needed to perform exercise tests on patients competently.Equipment,medications
,and personnel trained to provide cardiopulmonary resuscitation(CPR)
must be readily available. Although exercise testing of patients
is considered safe , there are reports of acute myocardial infarction
and death related to the procedure. Several surveys confirm
that up to 10 myocardial infarctions or deaths, or both, can
be expected per 10,000 tests.The risk is greater in postmyocardial
infarction patients and in those being evaluated for malignant
ventricular arrhythmias.
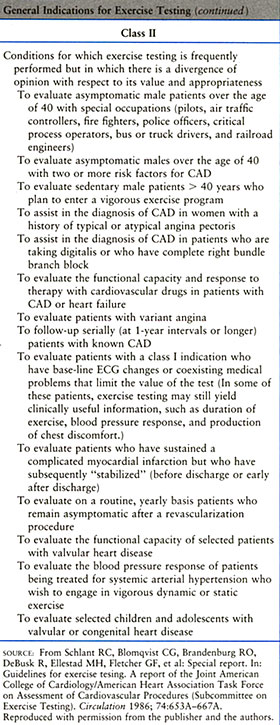
Figure 185 lists absolute and
relative contraindications to exercise testing |
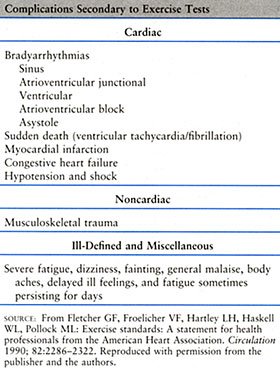
Figure 183 list three classes
of complications secondary to exercise tests. |
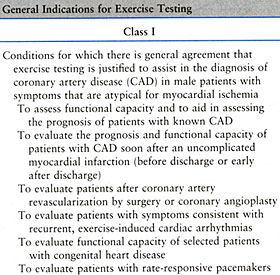
Figure 184 lists the general indications for exercise testing |
Good clinical judgement
is imperative in determining indications for and contraindications
to exercise testing. Whereas absolute contraindications are
quite definitive, in select cases with relative contraindications,even
submaximal testing may provide valuable information. The physician
should be certain that the subject understands the procedure
and acknowledges the risks. Good physician-patient communication
about testing and its risks is essential.
As stated in the American
Heart Association Exercise Standards, exercise testing of patients
should be performed under the supervision of a physician who
is trained to conduct exercise tests and who is responsible
for ensuring that the exercise laboratory is properly equipped
and that the testing personnel are appropriately trained.The
level or degree of supervision needed during a test is determined
by the clinical state of the patient being tested. Supervision
must be designated by the physician orphysician's staff, who
ask pertinent questions about the patient's medical history,perform
a brief physical examination,and review the standard 12-lead
ECG performed immediately before testing.The physician should
interpret data derived from testing, suggest further evaluation
or therapy, and aid in providing effective and timely advanced
CPR when necessary. A defibrillator and appropriate medications
should be immediately available.
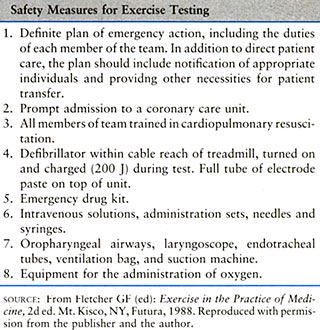
Figure 186 details
safety measures for exercise testing.
The degree of supervision
of an exercise test can range from assigning monitoring of the
test to a properly trained nonphysician(i.e.nurse or exercise
specialist) for testing apparently healthy younger persons(less
than 40 years old) or assigning patients with stable chest discomfort
syndromes to the physician who directly monitors blood pressure
and the patient's status throughout execise and recovery.The
latter is ideal for testing patients for diagnostic or prognostic
purposes and is a requirement for testing all patients at increased
risk for an exercise-induced complication.A physician should
be immediately available during all exercise tests on patients.
Patient Preparation
Preparatios for exercise
testing include the following:
1.The patient should
be instructed not to eat or smoke for 2 to 3 h before the test
and to dress appropriately for exercise. No strenuouos physical
efforts shoulb be performed for at least 12 h before testing.
2.Cessation of medications
may,at times, be considered since some drugs interfer with exercise
responses,complicating interpretation of execise testing. Most
patients are tested on their medications. Specific questioning
is important to detrmine which drugs have been taken so that
the physician can be aware of possible electrolyte abnormalities
and other effects.
3.A brief history
and physical examination should be done to rule out contraindications
to testing or to detect important clinical signs such as murmurs,
gallop sounds, pulmonary bronchospasm, or rales.Patients with
a history of increasing or unstable angina or uncontrolled heart
failure should not be have exercise testing until their condition
stabilizes.A cardiac physical examination should indicate which
patients have valvular or congenital heart disease,particularly
adult patients with severe aortic stenosis,who generally should
not undergo exercise testing.
4.A detailed explanation
of the testing procedure should be given,outlining risks and
possible complications.The patient should be told how to perform
the exercise test, and the testing procedure demonstrated.
5.A standard resting
12-lead ECG should be obtained since it differ from the resting
pre-exercise ECG.This is essential,particulaly in patients with
known heart disease,since an abnormality or a change may contraindicate
testing.Recording the ECG before starting the exercise test
and after hypervehtilation at another time may be helpful in
detecting false positive(indeterminate)ECG changes,particularly
in women.
6.Standing ECG and
blood pressure should be recorded to determine vasoregulatory
abnormalities, particularly ST depression.
EQUIPMENT AND
PROTOCOLS
The treadmill and
the cycle ergometer remain the most commonly used dynamic exercise
testing devices.
Protocols for clinical
exercise testing should include an initial low load (warm-up),
progressive uninterrupted exercise with an adequate duration
in each level, and a recovery period.
The most popular treadmill
protocol is the Bruce one.The advantages of the Bruce protocol
include a seventh or final stage,which cannot be completed by
most individuals, and its use in many published studies,which
provides extensive data for comparison.Its disadvantages include
large increments in work loads that make estimation of Vo2max
less accurate.In addition, the fourth stage can be either run
or walked,probably resulting in different oxygen costs.Some
subjects are forced to stop prematurely because of musculoskeletal
difficulties or inability to toleratethe high work load increments.Regardless
of technique used,the optimum exercise testing protocol should
last 6 to 12 min and should be adjusted to the type of patient
being tested.
Since there is strong
evidence that the level of exercise required to produce ischemia
is the most important part of the exercise test result,the question
arises of how the exercise test work load shall be selected.There
is overwhelming agreement on use of a progressive increasing
protocol beginning with a stage low enough to be tolerated by
the" weakest" candidate for testing and ending with
a stage sufficiently difficult to challenge "the fittest"
candidate.Each stage should be long enough in duration for the
subject to reach or closely approach steady state, and the the
work increments from one stage to the next should be small enough
topermit the desired degree of precision in estimating work
capacity.The Bruce treadmill protocol is widely used(figure
187).Typical work output requirements for each stage in terms
of oxygen consumption have been determined, and the range of
stages is adequate both for sedendary individuals and athletes.To
increase applicability, two easier stages may be added below
Stage1 in order to accommodate virtually all ambulatory individuals.
In order for measurements of of treadmill performance exercise
time, or rate-pressure response to be directly related to the
actual cardiac work involved, the subject must have reached
or closely approached "steady state". This implies
that if the subject continued to exercise at this intensity,cardiac
output,HR,and other indices would stay essentially the same
until the point of fatigue. Steady state attainment requires
at least 3 min, and perhaps longer on the treadmill, and exercise
times shorter than this will not yield a reliable reflection
of cardiovascular capacity.
Rather than assign
a certain stage of exercise protocol as a goal for an individual,it
is preferable to require the sibject to exercise progressively
through the protocol until it becomes excessively uncomfortable
or impossible to continue,i.e.,to an end-point of exhaustion
unless other terminating end-points occur. Failure to attain
an exercise tachycardia reasonably close to a predicted maximum
may not provide an adequate indication of the degree of effort
(figure 188).
SUBMAXIMUM
VERSUS MAXIMUM EXERCISE TESTING
Insomecases,testing
is terminated when the patient reaches 90% of predicted maximum
HR for age and level of training.The designated target HR, however,
may be maximal for some subjects ,beyond the limit of others,
but submaximal for others. A test is considered maximal when
the patient appears to give a true maximal effort(point of bodily
exhaustion) or when other clinical end-points are reached.
Indications for Terminating
Exercise Testing
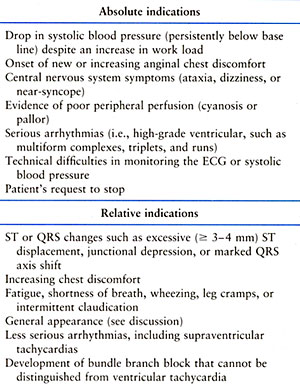
Indications for discontinuing
an exercise test include absolute and relative indications
(figure 189).
Some abnormal responses
occur only in recovery after exercise. For maximum sensitivity,
patients should be supine in the postexercise period. Monitoring
of Blood pressure and ECG should continue for at least 6 to
8min after exercise. An abnormal ECG response occurring only
in the recovery period is not unusual;these responses are likely
not false positive unless the occur late in recovery. Mechanicaldysfunction
andelectrophysiological abnormalities in the ischemic ventricle
after exercise can persist from minutes to hours.
INTERPRETATION
Clinical Responses
Classic ischemic chest
discomfort induced by the exercise test is strongly predictive
of CAD and is even more predictive in the presence of ST depression.
The patient's general appearance is also helpful.A decrease
in skin temperature,cool perspiration, and peripheral cyanosis
during exercise may indicate poor tissue perfusion due to inadequate
cardiac output with secondary vasoconstriction, and higher work
loads are not encouraged.Neurological signs such as light-headedness
or vertigo can also indicate inadequate cardiac output.
Physical examination
Cardiacexamination
immediately after exercise canprovide information about ventricular
functio.A percordial bulge or gallop rhythm can result from
left ventricular dysfunction.A mitral regurgitant murmur suggests
papillary muscle dysfunction related to transient ischemia.
Exercise or Functional Capacity
The maximal oxygen
consumption (V o2max) is the best index of maximal exercise
capacity. A decrease in maximum cardiac output may be a consequence
of CAD, and exercise may be limited by either anginal pain or
an acute reduction in LV output. An increase in LV diastolic
filling pressure and increasing pulmonary artery pressure will
also limit exercise. A mean exercise capacity of 10 MET's has
been observed in nonathletic middle-aged healthy men. If patients
with CAD reach 13 MET's, their prognosis is good, regardless
of other exercise test responses. As expected, patients with
an exercise capacity of less than 5 MET's have a higher mortality
during follow-up than patients with higher capacities.
A normal exercise
capacity does not exclude severe cardiac impairment. Mechanisms
proposed to explain a normal exercise performance in such patients
include increased peripheral oxygen extraction, preservation
of chronotropic reserve, ability to tolerate elevated pulmonary
wedge pressure without dyspnea, and increased levels of plasma
norepinephrine at rest and during exercise.
HEMODYNAMIC
RESPONSE
Blood pressure is
a function of cardiac output and peripheral resistance, Although
some normal subjects have a transient drop in systolic blood
pressure at maximum exercise, this finding is frequently associated
with severe CAD and ischemic dysfunction of the myocardium.
Exercise-induced hypotension also identifies patients at increased
risk for ventricular fibrillation in the exercise laboratory.
Figure 190 illustrates
normal and abnormal systolic blood pressure responses to exercise
tests.
A relatively rapid
HR during submaximum exercise or recovery could be due to vasoregulatory
asthenia, decreased vascular volume or peripheral resistance,
prolonged bed rest, anemia, or metabolic disorders and, therefore,
may not reflect intrinsic cardiac disease. This finding is also
relatively frequent in patients soon after myocardial infarction
or coronary artery surgery. A relatively low HR at any point
during submaximum exercise may due to lack of training or drugs
such as beta blockers. Conditions that affect the sinus node
can also attenutate the normal response of HR during exercise
testing.
Figure 191 shows predicted exercise HR in normals.
ECG Responses in Subjects with Normal
Resting Electrocardiograms
During exercise, the
P-wave vector tends to become more vertical and the P wave magnitude
increases in the inferior leads. The PR segments (intervals)
shortens and slopes downward in the inferior leads. The change,
which has been attributed to atrial repolarization (Ta wave),
may cause false-positive or indeterminate ST depression in the
inferior leads. Changes in R-wave amplitude are noted near maximum
effort with a decrease in the R wave in the lateral leads (V5)
at maximum exercise and 1 min into recovery. In the lateral
and veritical leads (V5 and and VF), the S wave becomes greater
in depth, showing a greater deflection at maximum exercise,
and then gradually returning to resting values in recovery.
The J-Junction is
depressed in the lateral leads at maximum exercise, then gradually
returns to pre-exercise values in recovery. A dramatic increase
in J-junctional depression may be observed in all leads and
may be greatest at 1 min into recovery. Subjects with resting
J-junction elevation may develop an isoelectric J-junction with
exercise as normal finding. These changes revert in recovery.
The normal ST segment vector response to both tachycardia and
exercise is a shift rightward and upward in the frontal plane;
however, there appears to be considerable biological variation
in the degree of this shift. A gradual decrease in T wave amplitude
is observed in all leads during early exercise. At maximum exercise
the T wave begins to increase, and at 1-min recovery the amplitude
is equivalent to resting values in the lateral leads.
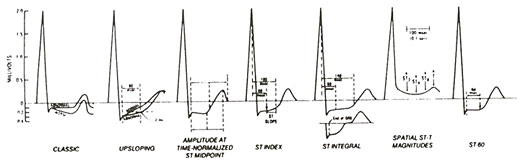
Abnormal Response
The ST-segment level
is measured relative to the PR segment since the U-P segment
usually is unclear during exercise. ST elevation is measured
as the deviation from the base-line ST level. If the base-line
ST segment is depressed, the deviation from that level to the
level during exercise or recovery is measured. The point for
measuring the ST level is the J-junction; points 60 to 80 ms
beyond this are usually used when the ST-segment slope is horizontal
or downsloping. Considering a rapidly upsloping ST depression
to be abnormal increases test sensivity but decreases specificity.
Various ST scores have been recommended, but none have been
validated as superior to standard "visual" measurements,
Exercise induced myocardial ischemia can result in one of three
ST-segment changes on the surface ECG; depression, elevation,
and normalization.
ST-segment depression
is the most common manifestation of exercise-induced myocardial
ischemia. It usually reflects diffuse subendocaridal ischemia,
with vector direction determined largely by the area of ischemia
and the placement of the heart in the thoracic cavity. The standard
criterion for this abnormal reponse is horizontal or downsloping
ST-segment depression of 0.10 mV (1.0 mm) or more for 80ms,
at least, three consecutive "isoelectric" or level
complexes.
As shown in figure 192, however,
other criteria have been considered.
Downsloping (divergent)
ST-segment depression usually reflects more ischemia than horizontal
depression. In the presence of base-line abnormalities (especially
in patients on digitialis), exercise-induced ST-segment depression
is less specific for ischemia. Factors related to the probablity
and severity of CAD included the degree, time of appearance,
duration, persistence in recovery, and number of leads with
ST segment depression. The lower the work load and the double
product at which the ST change occurs, the worse the prognosis
and the more likely the presence of multivessel CAD.
ST elevation must
be judged by whether or not it occurs in the presence of Q waves
from a previous myocardial infarction. ST-segment elevation
is more frequently observed in anterior leads (V1 and V2) with
Q waves.
Previous myocardial
infarction is the most frequent cause of ST-segment elevation
during exercise and seems to be related to dyskinetic areas
or ventricular aneurysms. Approximately 50 percent of patients
with recent anterior and 15 percent with inferior myocardial
infarction exhibit this finding during exercise. Patients with
elevation usually have a lower left ventricular ejection fraction
(LVEF) than those without such ST-segment elevation in leads
with abnormal Q waves from prior myocardial infarction. These
changes may result in reciprocal ST depression simulating ischemia
in other leads. The development of both ST-segment elevation
and depression during the same test may indicated multivessel
coronary artery disease (CAD).
In patients without
previous myocardial infarction (absence of Q waves on the resting
ECG), ST-segment elevation during exercise frequently reflects
severe transient ischemia resulting from significant proximal
CAD or spasm.
In patients with variant
angina, ST-segment elevation usually occur during spontaneous
anginal episodes, frequently at rest. During exercise, ST-segment
elevation had been reporte in about 30 percent of these patients
and a reversible thallium-201 perfusion defect usually corresponds
to the site of ST elevation. Another manifestation of ischemia
may be the normalization of an ST segment. ECG abnormalities
at test, including T-wave inversion and ST-segment depression,
may return to normal during attacks of angina and during exercise
in some patients with myocardial ischemia. This can also be
observed in subjects with a "persistent juvenille pattern"
on the resting ECG.
The R-wave amplitude
may increase during exericse in certain subjects with cardiac
disease; however, exercise-induced changes in R-wave amplituded
have not improved diagnostic accuracy despite use of several
lead systems, clinical subsets of patients, and different criteria
for an abnormal response.
In normal, a gradual
decrease in T wave amplitude is observed in all leads during
early exercise although the T wave begins to increase with maximum
exercise. At 1-min recovery, T-wave amplitude usually returns
to resting values. U-wave inversion may be associated with LV
hypertrophy, CAD, and aortic and mitral regurgitation. Exercise-induced
U wave inversion in patients with a normal resting ECG appears
to be a maker of myocardial ischemia and suggests left anterior
descending CAD. U-wave changes may, however, be diffucult to
assess during exercise, which increases HR and increases the
proximity of the T and P waves.
Plasma potassium increases
with maximal exercise testing and increases more after training
in subjects on atenolol and propanolol therapy. In addition
(in sedentary individuals), both plasma potassium and magnesium
increase significantly with maximal exercise, and these increase
are unaffected by atenolol and propranolol blockade. To the
contrary, propranolol, but not atenolol and placebo, prolongs
the time of return to base line of potassium (compared to magnesium)
after the acute exercise. Such changes must be considered with
exercise testing because of electrolyte effects on ST, T, and
U waves.
Exercise tests can
be performed with radionuclide imaging to further evaluate myocardial
perfusion. Echocardiographic images and Doppler flow measurements
can also be made during and after exercise, and LV EF, wall
motion, and valvular function can be assessed with these techniques.
DIAGNOSTIC
VALUE OF EXERCISE TESTS
Sensitivity and Specificity
The sensitivity and
specificity are terms used to define how effectively a test
detects disease. Sensitivity is the percentage of those with
a disease who will have an abnormal test. Specificity is the
percentage of those without the disease who will have a normal
test. This may be affected by drugs, baseline E C G patterns,
and whether a test is submaximal or maximal. Sensitivity and
specificity are inversely related ;when the sensitivity is the
highest, the specificity is the lowest and vice versa.
If the population
studied has a greater prevalence of disease, the test will have
a higher sensitivity. For instance, the exercise test has a
higher sensitivity in individuals with triple vessel CAD than
those with single-vessel disease. A test can also have a lower
specificity if it is used in individuals who are more likely
to give false positive (indeterminate) results such as women
or individuals with mitral valve prolapse.
Sensitivity and specificity
of exercise-induced ST segment depression can be demonstrated
by comparing the results of exercise testing and coronary angiography.
In these studies the exercise tests with 0.1 mV horizontal or
down sloping ST depression has approximately 84 percent specificity
for angiographically significant CAD; that is 84 percent of
those without significant angiographic disease had a normal
exercise test.These studies had a mean 66 percent sensitivity
of exercise testing for significant angiographic CAD , with
the range from 40 percent for one vessel disease to 90 percent
for three- vessel disease
PROGNOSTIC USE OF THE EXERCISE TEST
The two major reasons
for determining prognosis are to provide reliable answers about
the probable outcome of the cardiovascular illness and to identify
patients in whom interventions might improve the eventual outcome.
Figure 193 lists indications
for performing an exercise tests in patiens after myocardial
infarction.
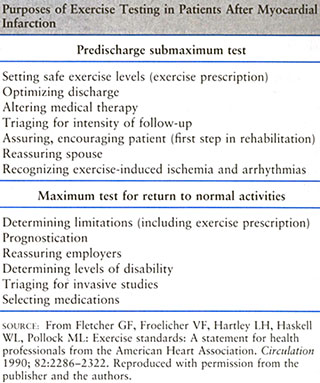
Exercise testing may
be appropriate and expedite hospital discharge of patients recovering
from a myocardial infarction. Ventricular arrhythmias not present
at rest may be provoked during exercise and the patient's reaction
to exercise at the time of discharge from the hospital can be
assessed. An exercise test before discharge is important for
providing guidelines for activity at home, reassurance of physical
status, determination of risk of complications, and to provide
a basis for advising the patient to resume or increase activity
level and return to work.
Some investigators
perform exercise tests using symptom-or sign- limited end points
two to the three weeks after myocardial infarction. In many,
the submaximal limited test is quite appropriate. The heart
rate limit of 130 to140 beats per minute and a MET of five to
seven is arbitrarily used, and a Borg perceived exertion level
in the range of thirteen to fifteen can be used as an end point,
particularly for patients receiving beta blockers. The maximal
test is probably more appropriate three of more weeks after
myocardial infarction, when the patiens is more often ready
to assume full activities.
One review of numerous
predischarge and postmyocardial infarction exercise tests reported
a few serious complications: two cases of recurrent infarction
and two cases of ventricular fibrillation, one fatal,representing
0.05% morbidity and 0.0 2% mortality. In studies of exercise
testing after myocardial infarction with a follow-up for cardiac
end-points, tested patients consistently had a lower risk, regardless
of criteria used for testing. Of the usual general criteria,
only an abnormal systolic blood pressure response or a low exercise
capacity were significantly associated with poor outcome. When
thestudies were subgrouped by whether testing was done before
or after discharge from the hospital, a high proportion of the
predischarge test results indicated poor outcome. Submaximal
testing resulted in the highest proportion of positive associations
and the highest risk ratios, and abnormal response at higher
workloads were not as predictive as those at lower workloads.
Studies using exercise
testing of the patiens with stable CAD have provided data to
predict angiographic findings, cardiac events and those with
silent ischemia, or improved survival with coronary artery bypass
surgery(CABS) .
Exercise testing has
been used to predict left main or triple vessel coronary artery
disease, or both, with varying results.
Exertional Hypotension
In most studies,
exercise- induced hypotension indicates a poor prognosis, and
has a predictive value of up 50 percent for left main/triple
vessel disease. Exercise induced hypotension can occur in patients
with CAD, valvular heart disease, or cardiomyopathy. Occasionally,
however, subjects without clinically significant heart disease
will exhibit exercise induced hypotension during exercise related
to antihypertensive therapy or prolonged strenuous exercise.
Cardiac Events in Patients with
the Silent Ischemia
The prognostic implication
of asymptomatic(" silent") ischemia detected during
exercise testing is controversial. It has been suggested that
those with silent ischemia are at greater risk of cardiac death;
however, in three large studies of patients with a high prevalence
of CAD who underwent exercise testing, those with ST-segment
depression, with or without angina during testing,had similar
prognoses. Ischemia is asymptomatic in approximately 60 percent
of patients with CAD and ischemic ST-segment depression and
silent ischemia occurring with treadmill testing does not appear
to confer an increased risk for death relative to patients experiencing
angina with signs of ischemia.
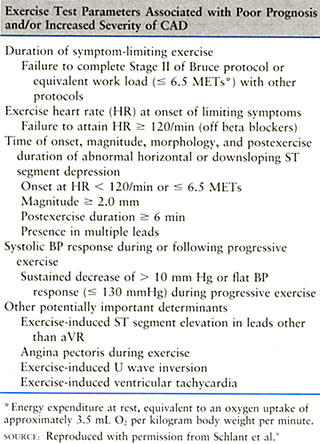
Figure 194 itemizes
exercise testing findings associated with a poor prognosis in
patients with CAD
and figure 195 shows
data from eight studies in the prediction of cardiac events.
In patients with
CAD, exercise-induced ventricular arrhythmias are not an independent
risk factor for subsequent mortality or coronary events.Some
studies, however ,suggests that these arrhythmias may add independent
prognostic information to thallium-201, ST-segment, and heart
rate changes and are associated with severe CAD and wall motion
abnormalities. In selected subjects with CAD, exercise testing
may be of considerable value in the evaluation of drug therapy
of ventricular arrhythmias.
One study suggests
that patients with multi- vessel CAD, cardiomegaly, exercise
capacity of less than 5 METS,or a maximum systolic blood pressure
of less than 130 mmHG.do better with surgery.In another trial,patients
who had an exercise test response of 1.5 mm of ST-segment depression
or claudication.In another study. the benefit of surgery was
greatest in patients with 1 mm ST-segment depression at less
than 5 METS.
In several studies
that evaluated graft occlusion and reoccurrence of symptoms,
exercise- induced ST depression did not predict prognosis after
coronary artery bypass surgery. An exercise capacity of nine
mets or more, however, indicates a good prognosis, regardless
of other responses.
Exercise testing
may be of value in the routine( six to twelve month) follow
up with patients who have undergone percutaneous coronary angioplasty,
especially in evaluation of chest discomfort and detection of
restenosis. Testing is ofparticular benefit in patients in cardiac
rehabilitation programs. It may be especially helpful in the
patient with symptoms suggested of ischemia or the patient whose
progress in rehabilitation is limited.
There is substantial
support for the use of exercise testing as the first noninvasive
procedure after the history, physical examination, and resting
ECG in the prognostic evaluation of patients with coronary artery
disease. Exercise testing accomplishes both purposes of prognostic
testing by providing information about the patient's clinical
status and in helping provide recommendations for proper management.
Exercise testing also helps select patients who should undergo
further evaluation such as radionuclear studies and coronary
angiography. Since the exercise test can be performed as an
outpatient patient procedure and provides valuable information
about activity levels, response to therapy,and disability ,
it is a reasonable first choice for prognostic assessment. Because
of its widespread availability ,the exercise test can have an
enormous impact on cost- effectiveness delivery of cardiovascular
care. The exercise test is not usually recommended for screening
apparently healthy persons without risk factors since it has
a high rate of false positive results.
OTHER USES
OF THE EXERCISE TEST
Exercise testing
has been used in patients with a valvular heart disease to evaluate
exercise- induced symptoms to quantitative disability, and to
evaluate the response to medical and surgical therapy. It has
also been used to identify a concurrent coronary artery disease;
however, there is a high prevalence of false positive responses
because of frequently seen baseline ECG abnormalities and left
ventricular hypertrophy .
In selected patients
with valvular heart disease exercise, testing may be useful
to determine when surgery indicated .Effort syncope in patients
with aortic stenosis is an important symptom. Most guidelines
for exercise testing list moderate to severe aortic stenosis
as a contrindication for testing because of concerns about syncope.
and cardiac arrest. Therefore, exercise testing of patients
with the aortic stenosis should be restricted to patients with
mild to moderate gradients. Four proposed mechanisms for exercise-
induced syncope in patients with the aortic stenosis include
carotid hypersensitivity, left ventricular failure,arrhythmias,
and left ventricular Baroreceptor stimulation. Exercise testing
,however, is relatively safe in both the pediatric and adult
patient with mild to moderate aorticstenosis when performed
very carefully and with experienced supervision. Attention should
focus on the patient's symptoms, minute by minute response of
blood pressure, slowing heart rate, and both ventricular and
atrial arrhythmias.In the presence of an abnormal blood pressure
response, the patient with a aortic stenosis should take at
least a two minute cool- down walk at a lower stage of exertion
to avoid acute left ventricular volume overload, which may occur
when the patient assumes the supine position
Patients with aortic
regurgitation usually maintain a normal exercise capacity for
a longer period of time than those with the aortic stenosis,
as volume workload of the myocardial requires less oxygen and
pressure work. During exercise, there is a decrease in the diastolic
duration and regurgitant volume and a decrease in vascular peripheral
resistance, favoring forward output. As the myocardium fails,both
the left ventricular ejection fraction and stroke volume decrease
with an increase in both end-diastolic and and end-systolic
ventricular diameter. Exercise testing is usable for monitoring
selected patients with aortic regurgitation, using the appearance
of the ST- segment depression, a reduction in heart rate response
to each workload ,and a decrease in Vo2 max as markers for decreasing
left ventricular function.
Patients with mitral
stenosis may have either a normal or excessive increase in heart
rate during exercise. As stroke volume cannot be increased,
the usual increase in cardiac output is less and may eventually
fall during exercise, frequently accompanied by exercise- induced
hypotension. The increase in heart rate and right ventricular
pressure results in an increase in right ventricular myocardial
oxygen demand. In patients with mitral stenosis chest discomfort
and ST- segment depression during exercise may occur either
due to coronary artery disease or secondary to pulmonary hypertension.ST
depression during exercise is attributed both to a decrease
incoronary perfusion secondary to tachycardia and a fall in
cardiac output and to an increase in myocardial oxygen demand
secondary to right ventricular overload. The shortening of diastole
associated with tachycardia and the increase in pulmonary blood
flow associated with exercise increase left atrial pressureand
may cause pulmonary congestion.
Patients with mild
to moderate mitral regurgitation maintain normal cardiac output
during exercise. Blood pressure, heart rate, and ECG responses
are usually also normal. When transient mitral regurgitation
occurs suddenly during exercise as a result of ischemic papillary
muscle dysfunction, however, a flat response in systolic pressure
can occur. Patients with severe mitrall regurgitation usually
have decreased cardiac output and limited exercise capacity.
ST-segment depression during exercise is infrequent in these
patients; however, a hypotensive response can develop, and arrhythmias
arefrequent.
Several mechanisms
have been suggested to explain the ST depression noted in some
patients with mitral valve prolapse including regional ischemia
of the papillary muscle, coronary artery disease, compression
of the anterior descending artery, coronary spasm, and primary
cardiomyopathy.ECG ST changes can be normalized by propranolol
or other nonselective beta blockers, improving the specificity
of the exercise test.
An exercise test
is often used to evaluate the safety of an exercise training
program and to formulate an exercise prescription. In general,
an exercise test is useful for a sedentary individual who at
the age of 40 decides to enter an exercise program of a higher
intensity than walking at 50 to 60 percent of maximum heart
rate reserve. Testing should also be done in younger individuals
with coronary risk factors or a strong family history of coronary
artery disease. It is preferable to determine an individual's
maximum heart rate rather than give a predicted value for maximal
heart rate to be attained during training, because of the wide
scatter of maximum heart rate when plotted against age An exercise
test can be used in adult exercise or cardiac rehabilitation
programs to safely advance an individual to a higher intensity.
An improvement in exercise capacity on an exercise test can
also be an effective incentive to continue the program and to
encourage risk factor modification.
Exercise testing
is used to determine the degree of impairment and disability
of patients with various forms of heart disease. Patients who
"exaggerate" their symptoms who have a psychological
impairment can often be identified.Vo2max is the best none invasive
measurement of exercise capacity of the cardiovascular system.
Inability to reach five METS without symptoms or signs is a
criteria of disability used by the social security administration.
The determination of the patient's exercise capacity affords
an objective measurement of the degree of cardiac impairment
The results of exercise
testing do not add significantly to the risk stratification
provided by the resting the ECG in patients without known coronary
artery disease or candidates for major elective noncardiac surgery.
Therefore, exercise testing is not routinely recommended before
elective noncardiac surgery under general anesthesia.The efficacy
of angioplasty or surgery for peripheral vascular disease can
be assessed by exercise testing.
Fletcher,G.F.,M.D. and Schlant,R.C.,The
Exercise Test,Hurst's The Heart,8th Edition,P.423-440.
DRUGS AND EXERCISE TESTING
Beta Blockers
Maximun heart rateand
systolic blood pressure product during exercise may be reduced
by beta blockers. Patients with angina who receive beta blockers
may have a greater exercise capacity with less ST-segment depression
and less ischemia if the drug prevent their reaching the ischemic
rate product.In some patients, however, angina disappears, but
the ST depression occurs if th e ischemic product can still
be reached.
Vasodilators
Vasodilators can
increase exercise capacity in patients with angina or heart
failure, or both. To date, however, there's no good data that
long acting nitrates increase exercise capacity in patients
with angina when they are tested after chronic administration.
Angiotensin converting enzyme inhibitors
Angiotensin converting
enzyme inhibitors decrease the blood pressure both at rest and
duringI exercise and can increase exercise capacity in patients
with chronic heart failure.
Calcium Antagonists
Calcium antagonists
have multiple hemodynamic effects.. They can delay time to ischemia,improve
exercise capacity, delay ST-segment depression until higher
work loads.Heart rate and systolic blood pressure are decreased
for a given level ofexercise.
Digitalis
ST-segment depression
can be induced or accentuated during exercise in individuals
are taking digitalis, including normalsubjects and patients
with CAD.Profound ST-segment depression(Greater than2mm more)
compared to baseline usually indicates ischemia, even in patients
who are taking digitalis.The exercise induced ST-segment depression
related to digitalis has been said to persist for 2 or more
weeks after digoxin is discontinued.
Other drugs
Quinidine can cause
prolongation of phase 2 of the ventricular action potential,
decreasing the repolarization gradient during the ST segment
and thus decreasing the magnitude of the ST depression. A decrease
of twenty beats per minute in maximum exercise heart rate has
been reported in patients taking amiodarone .Amiodarone also
increases duration of QRScomplex during exercise. Diuretics
can cause hypokalemia,producing muscle fqtigue ventricular ectopy
,and rarely ST segment depression with exercise.
Fletcher,G.F.,M.D. and Schlant,R.C.,The
Exercise Test,Hurst's The Heart,8th Edition,P.423-440.
SPECIAL CASES
OF EXERCISE TESTING INTERPRETATION
A relatively low heart
rate at any point during submaximal exercise may be due to lack
of training or drugs such as beta blockers.
Conditions that affect
the sinus node can also attenuate the normal response of heart
rate during exercise.First-degree atrioventricular(AV)block
occasionally occurs at end of exercise or during recovery phase.Medications
or conditions that may produce prolonged AV conduction time
(e.digitalis, propanolol, myocarditis) may also predispose the
individual to lengthing of the PR interval. Second degreeAV
block-Wenckeback(Mobitz 1) during exercise is rare.Mobitz type-2
AV block has been seen in patients with CAD.
Exercise may induce
cardiac arrhythmias under several conditions,especially diuretic
and digitalis therapy.The recent ingestion of alcohol or caffeine
may also exacerbate exercise-induce arrhythmias.CAD(coronary
artery disease) can predispose some patients to arrhythmias
during exercise.
Ecotopic ventricular
beats(PVC's) are the most frequent typed cardiac arrhythmia
that develop during exercise, followed by supraventricular arrhythmias.Their
prevalence is directly related to age and cardiac abnormalities.In
general,ectopic ventricular contractions are of concern in patients
with a family history of cardiomyopathy, valvular heart disease
or known severe ischemia.
Sinus arrhythmias
with periods of sinus bradycardia and a wandering atrial pacemaker
are relatively common during exercise and the immediate recovery
phase.Atrial ectopy can occur in normal or diseased hearts.Exercise-induced
transient atrila fibrillation and flutter occur in less than1%
of individuals who undergo exercise testing.These arrhythmias
may be induced by exercise in both healthy individuls and patients
with rheumatic heart disease, hyperthyroidism,WPW syndrome,or
cardiomyopahty.Exercise induced supraventricular arrhythmias
alone are usually not related to CAD, but are more often related
to pulmonary disease ,recent alcohol ingestion, or excessive
caffeine.
Fletcher,G.F.,M.D. and Schlant,R.C.,The
Exercise Test,Hurst's The Heart,8th Edition,P.423-440.
Blood Pressure Response
Systolic blood pressure should
rise with increasing treadmill workload, whereas diastolic blood
pressure usually remains about the same (Fig.181 ). A rising
diastolic blood pressure can be associated with coronary heart
disease: however, it ismore likely a marker for labile hypertension,
which leads to coronary disease. A drop in systolic blood pressure
below preexercise values is the most ominous criterion, whereas
a drop of 20 mmHg or more without a fall below preexercise values
appears to have less predictive value. Exercise-induced hypoten-sion
(EIH) can be due to either left ventricular dysfunction (as
reflected by myocardial infarction status), ischemia, or outflow
obstruction. When EIH occurs without association with either
of these two factors, EIH appears to be benign.
The highest systolic blood pressure should be achieved at maximal
workload. When exercise is stopped, approximately 10 percent
of people tested will abruptly drop their systolic blood pressure
owing to peripheral pooling. To avoid fainting, patients should
not be left standing on the treadmill. The systolic blood pressure
usually normalizes on resuming the supine position during recovery
but may remain below normal for several hours after the test.
Irving et al. examined variations in clinical noninvasive systolic
pressure at the point of symptom-limited exercise on a treadmill.
Lower maximal systolic pressures often were associated with
two- or three-vessel disease or reduced ejection fraction or
both. The annual rate of sudden cardiac death decreased from
98 per 1000 men to 25 and 7 per 1000 men as the range of maximal
systolic pressure increased from less than 140 to 140 to 199
to 200 mmHg or more, respectively.
The 3-min systolic blood pressure ratio is a useful and readily
obtainable measure that can be applied in all patients who are
undergoing exercise testing for the evaluation of known or suspected
ischemic heart disease . The ratio is calculated by dividing
the systolic blood pressure 3 min into the recovery phase of
a treadmill exercise test by the systolic blood pressure at
peak exercise. A 3-min systolic blood pressure ratio greater
than 0.90 is considered abnormal. Higher values for the ratio
are associated with more extensive coronary artery disease,
as well as an adverse prognosis after myocardial infarction.