Ventricular
fibrillation (see figure 9B) is a terminal arrhythmia, uniformly
requiring rapid initiation of emergency measures.
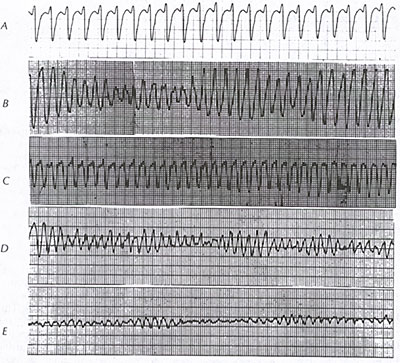
Ventricular
flutter(see figure 9B) with loss of consciousness and rapid
unstable VT may be clinically equivalent to VF and is treated
identically when accompanied by the clinical picture of cardiac
arrest. Ventricular fibrillation occurs commonly in the setting
of acute ischemic events (see figure 70) or unpredictabley in
advanced chronic ischemic heart disease. Moreover, it is the
mode of death in 25 to 50 percent of fatalities among patients
with cardiomyopathies (see figures 39A, 39B, 39C, 39D, 39E,
39F, 39G, 43B, 73, 74, 75, 76, 77A, 77B) . It may also develop
during hypoxia, atrial fibrillation with rapid ventricular responses
in WPW syndrome (see figure 3A, 3B), R-on-T pacing or cardioversion,
or improper grounding of electrical devices or as proarrhythmic
(see figure 13) effects of antiarrhythmic drugs. A particularly
high risk setting for VF is acute myocardial infarction with
right or left bundle branch block.
Ventricular fibrillation
may occur de novo, but among patients with out-of –hospital
cardiac arrest, VT commonly precedes the onset of VF.
The right coronary artery is a common site of isolated coronary-artery
spasm leading to cardiac arrest due to ventricular fibrillation
(figure 9d).
The
electrocardiographic pattern of VF is that of gross disorganization
without identifiable repetitive waveforms or intervals (see
figure 9B). At the onset, VF may be “coarse” in pattern, but
over time, it loses its amplitude and becomes “fine” (<0.2 mV)
(see figure 9B, parts D and E). Successful defibrillation and
survival rates are decreased in patients with the fine pattern
of VF (see figure 9B, part E). In ventricular flutter, a sine
wave configuration is present, having a cycle length in the
range of 200 to 240 ms (see figure 9B, part C). Rapid polymorphic
VTs may be difficult to distinguish from ventricular fibrillation
or flutter.
MALFUNCTION
OF INTERNAL CARDIOVERTOR DEFIBRILLATORS
Here are devices currently available, incorporating both the
pacemaker(VVI pacing) as well as the implantable cardioverter
defibrillator to treat those patients with a history of chronic
sinus bradycardia,A-V conduction system disease,or severe postshock
bradyarrhythmias.
The malfunctioning ICD may be caused by lead fracture or migration,premature
battery depletion,and generator malfunction.
All units usually are modified temporarily by placing a magnet
over the pulse generator.Tachycardia detection and therapy are
temporarily suspended by magnet placement.
Appropriate ,undesirable discharges may sometimes be difficult
to distinguish from appropriate,desirable shocks(atrial fibrillation
with a rapid ventricular rate exceeding the programmed rate
cutoff may trigger an appropriate (although undesirable)discharge
and may account for repetitive discharges experienced in close
succession.
Devices with second look features that require arrhythmia reconfirmation
immediately prior to shock delivery have largely eliminated
the problem of undesirable discharges due nonsustained ventricular
tachycardia.Sensing lead malfunction( oversensing) resulting
from lead fractures may be the cause of inappropriate discharges
triggered by sensing artifact.
Lead disruption may be diagnosed on the basis of over pentrated
x'ray findings,by analyzing audible tones emitted in synchrony
with the sensed events, or examing the telemetered records of
stored or real-time intracardiac electrograms.Discharge during
sinus rhythm is strong evident for sensing malfunction.Analysis
of electrograms or rate intervals recorded by the newer devices
during sinus rhythm and at time of therapy has allowed for better
correlation between arrhythmic events and device responses and
has greatly facilitated the diagnosis of lead or pulse generator
malfunction.
In suspected pacemaker malfunction in cases with the pacer
as well as the ICD,long strips of several ECG leads should be
taken.The ECG must be recorded in the base (synchronous) and
magnet(asynchronous) modes.Because of competitive rhythms when
using a magnet, most manufacturers use a magnet rate between
90 and 100 pulses per minute to override spontaneous rhythms.With
single chamber pacing systems the ECG in the synchronous or
asynchronous modes should confirm normal pacing,The stimulus
artifact of the bipolar lead system is often impossible to see
on the surface ECG.In these cases.polarity programming with
verification of pacing in the unipolar mode is very useful.For
confirmatiom of pacemaker sensing in patients with consistent
pacing,the patient can be exercised to accelerate the intrinsic
rate or the pacing rate reduced by programming until the intrinsic
rate emerges.
The runaway pulse generator of the pacemaker is a rare problem(referring
to an increase in pacing rate beyond 150 pulses/minute with
sufficient output to capture the heart).