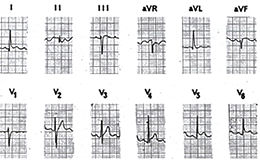
Figure 35c
click
to enlarge
Acute viral and idiopathic pericarditis is a disease in which there is an inflammation of the pericardium, the thin fibrous covering of the heart (figures 27).
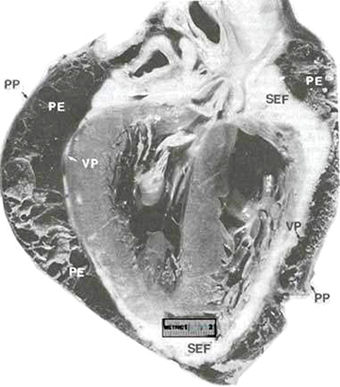
Fig. 27
Fibrous pericardial effusion (PE) helps to delineate the two normal layers of the pericardial sac: visceral pericardium (VP) and parietal pericardium (PP).
Subepicardial fat (SEF) is located just beneath the visceral layer of pericardium.
B.F. Waller and R.C. Schlant: Anatomy of the Heart: Hurst's The Heart, 8th ed, p 76.
The chest pain is relieved by sitting up and may be aggravated by breathing. The rub sounds superficial, scratchy, and creaky over the heart (the left chest).
In some cases there is fever.
Causes include the following:
1) viruses, especially the coxsackie B5, B6 and the echovirus,
2) indirect trauma to the chest,
3) blows to the chest,
4) surgical procedures,
5) bacterial infections,
6) tumors,
7) Dressler’s post myocardial infarction syndrome,
8) myocardial infarction (inflammation occurring after a heart attack)
9) medications.
Treatment includes analgesics, anti-inflammatory agents, such as motrin. Specific causes, if known, can be treated.
RECURRENT PERICARDITIS
Recurrent or relapsing acute pericarditis
is one of the most distressing disorders of the pericardium
for both patient and physician; it may occur with or without
pericardial effusion and occasionally is associated with pleural
effusion or parenchymal pulmonary lesions. Recurrences occur
with highly variable frequency over a course of many years.
The reasons for relapse are unclear, but the phenomenon suggests
that acute pericarditis itself may represent or generate an
autoimmune process. Recurrences may be spontaneous but more
commonly are associated with discontinuation or tapering doses
of anti-inflammatory drugs. When associated with pericardial
effusion, relapsing pencarditis can cause cardiac tamponade;
however, this is unusual.
Painful recurrences of pericarditis may respond to nonsteroidal
anti-inflammatory agents but commonly require corticosteroids.
Once steroids are administered, dependency and the development
of steroid-induced abnormalities are potential sequelae. Prednisone
is begun at a high dose (60 to 80 mg/day), but rapid tapering
should be initiated within a few days of clinical resolution.
When necessary, the risks of long-term steroids should be minimized
by using the lowest possible dose, alternate-day therapy, combinations
with nonsteroidal drugs, or coichicine (etc 2 mg/day). In the
most difficult cases, relapse occurs every time the dose of
prednisone is reduced below 5 to 20 mg/day. When this occurs,
the patient should be maintained for several weeks on the lowest
suppressive dose before the next taper commences. Azathioprine
(50 to 100 mg/day) also has been used to prevent recurrent episodes.
Although encouraging results have been reported in a series
of patients who underwent pericardiectomy for recurrent pericarditis,
pencardiectomy may simply abbreviate rather than terminate the
painful recurrences. Thus, pericardiectomy should be considered
only when repeated attempts at medical treatment have clearly
failed.