(Regurgitation)
This is a condition in which the aortic valve
has become disfigured to such an extent that its leaflets no
longer are able to completely oppose each other during diastole
(see figures
48a,
48b,
48c,
48d).
This condition allows blood to flow back
into the left ventricle from the ascending aorta during diastole
(figures
48i, 48j,
48k).
Normally, there is no leakage of blood from the ascending aorta
back into the left ventricle after systole.
Aortic valve regurgitation can be caused by
infection of the aortic valve due to syphilis via unprotected
coitus, (figure 205 immediately below) and bacteria, which have
gained access to the blood stream and the aortic valve through
the use of illicit drugs intravenously.
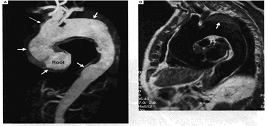
Figure 205
Examination of a 74-year-old man with a one-year
history of mild, stable angina revealed a murmur consistent
with the presence of aortic regurgitation. Echocardiography
demonstrated severe aortic regurgitation as a result of marked
dilatation of the aortic root (diameter, 5.4 cm in the proximal
ascending aorta). Gadolinium-enhanced magnetic resonance
angiography (Panel A) revealed saccular dilatation of the aorta
from its root to beyond the distal arch (short arrows), with
involvement of the innominate artery (long arrow). T1-weighted
images also revealed evidence of mural thrombus in the superior
aspect of the aneurysm, beyond the left subclavian artery (arrow
in Panel B). Serologic immunofluorescence studies revealed the
presence of Treponema pallidum antigen, confirming the clinical
suspicion of syphilitic aortitis and aneurysm. The patient received
10 days of intramuscular penicillin G procaine with oral probenecid
without complications, and he continues to receive medical therapy
under close surveillance.
The cardiovascular complications of syphilis predominantly involve
the aorta, leading to the formation of aneurysms and aortic-valve
incompetence. Angina may result from coronary ostial stenosis
or associated atherosclerosis. The incidence of tertiary syphilis
has declined in recent decades owing to the early recognition
of the disease and the sensitivity of the pathogen to antibiotics.
However, the reemergence of syphilis in the developing world,
particularly among drug abusers and the sexually promiscuous,
may mean that the delayed cardiovascular and neurologic complications
of late syphilis will be seen with increasing frequency.
Pugh,P.J.andGrech,E.D.,N
Engl.Med,Vol.346,No.9,P.676,Feg.28,2002.
These infections may also be caused by bacteria
gaining access to the blood stream from dental procedures.
Certain congenital abnormalities such as bicuspid
aortic valve (see figure
23b) and disorders of connective tissue as well as rheumatic
heart disease (see figure
48b,
111), inflammation of the aorta (Takayasu), high blood pressure,
arteriosclerosis, infective endocarditis (see figure
48c,
48e,
48f), following prosthetic valve surgery including fungus
infection (see above figure 48g), cystic medial necrosis of
aorta are some of the causes of aortic regurgitation.
Myxomatous Aortic Valve Prolapse
The aortic valve has three cusps (right and
left coronary ones and a noncoronary one). In the case of myxomatous
cusps ,there is the finding histologically of a marked increase
in the delicate myxomatous connective tissue between the aortic
surface (thick layer of collagen and elastic tissue forming
the the aortic aspect of the cusp) and the fibrosa or ventricularis,
which is composed of dense layers of collagen and forms the
basic support of the cusp.This myxomatous proliferation of the
acid mucopolysaccharide-containing spongiosa tissue causes focal
interruption of the fibrosa. Secondary effects include fibrosis(scarring)
of the surfaces of the cusps, and ventricular friction lesions.The
valves become redundant and scalloped.
Aortic valve prolapse occurs in 2 % of patients
with mitral valve prolapse(MVP).The primary form of MVP may
occur in families,where it appears to be inherited as an autosomal
dominant trait with varying penetrance. It can also occur in
isolated cases.MVP has been found with incresing frequency in
patients with Marfan syndrome.
MVP is commonly associated with thoracic skeletal
abnormalities such as the straight spine and pectus excavatum.
Some have postulated that MVP results from
fetal exposure to toxic substances during the early part of
pregnancy.
Management of Aortic Insufficiency
All patients with AR need antibiotic prophylaxis
to prevent infective endocarditis. Patients with AR of a rheumatic
origin need antibiotic prophylaxis to prevent recurrences of
rheumatic carditis. Patients with syphilitic AR need a course
of antibiotics to treat syphilis.
Patients with mild AR need no specific therapy (
Table 1 ). They do not need to restrict their activities
and can lead a normal life. Patients with moderate AR also usually
need no specific therapy. These patients, however, should avoid
heavy physical exertion, competitive sports, and isometric exercise.
The value of long-term vasodilators to produce an improvement
in LV size and function has been evaluated in two placebo-controlled
randomized trials. In the hydralazine trial, 36 percent of the
patients were in NYHA functional class II, and patients had
moderate to severe AR. Hydralazine produced modest reduction
of LV end-diastolic volume and a small increase in ejection
fraction at the end of 2 years; however, because of side effects,
long-term compliance was poor, which probably accounted for
the extremely modest beneficial effects. In asymptomatic patients
with severe AR, a calcium channel blocking agent, long-acting
nifedipine, produced significant reductions in blood pressure
and LV end-diastolic volume and mass and major increases in
LV ejection fraction at the end of 1 year. Almost all patients
completed the trial. Recently, a prospective randomized trial
in asymptomatic patients with normal LV systolic function showed
that at the end of 6 years, 34 ± 6 percent of patients
treated with digoxin developed LV systolic dysfunction and/or
symptoms and thus needed valve replacement, compared to 15 ±
3 percent of patients treated with long-acting nifedipine (p
< .001) (
Fig. 48l ); 90 percent (23 of 26) of those who needed valve
replacement had developed LV systolic dysfunction with or without
symptoms; only 3 had become symptomatic without developing LV
systolic dysfunction. Accordingly, all asymptomatic patients
with severe AR and normal LV systolic function should be treated
with a vasodilator (calcium antagonists long-acting nifedipine)
unless there is a contraindication to its use.
The role of nifedipine in patients with moderate AR has not
been studied. In view of its beneficial effects in severe AR,
long-acting nifedipine could be used in selected patients with
moderate AR if there are no contraindications to its use. An
acute study showed that nifedipine was superior to an ACE inhibitor,
and a 6-month trial showed that the results with captopril were
similar to placebo. One study with quinapril involved 10 patients,
many of whom had moderate AR.In another study with enalapril,
most patients had mild to moderate AR and many had severe systemic
hypertension.Moreover, there are no published data to show that
ACE inhibitor therapy reduces the need for valve surgery. In
brief, ACE inhibitors are not of proven benefit in asymptomatic
patients with AR and with normal LV systolic function.
Symptomatic patients with severe AR need medical and surgical
treatment. Medical treatment ( Table 1 below ) consists of the
administration of digitalis, diuretics, and vasodilators. Digitalis
acts by increasing myocardial contractility, often reducing
LV end-diastolic volume while increasing the LV ejection fraction
and also the cardiac output if it is reduced in the resting
state. Digitalis is clearly indicated in patients with symptoms.
TABLE 1 Medical Treatment of Patients
with Aortic Regurgitation
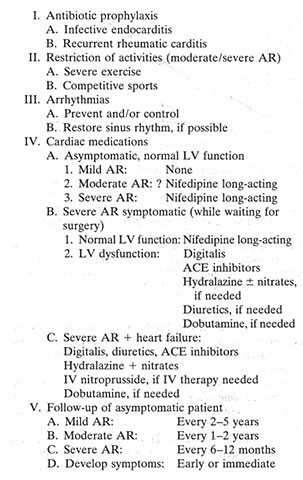
SOURCE: Copyright © by S. H. Rahimtoola,
M.B., F.R.C.P., M.A.C.P., MA.C.C. See Ref. 93.
The need for and benefits of this therapy
in asymptomatic patients have not been well documented. Diuretics
are of value when the left atrial pressure is elevated and in
the presence of heart failure.
Vasodilators are either arterial, venous, or both. Vasodilators
act by reducing the peripheral arterial resistance, which favors
forward cardiac output and reduces regurgitant volume; initially,
the total LV stroke volume remains unchanged. If the left atrial
pressure is elevated and LV ejection fraction reduced, vasodilators
frequently result in an improvement in both.
Long-term hydralazine therapy in symptomatic patients resuits
in significant benefit in only 20 to 35 percent of patients.Those
who are likely to benefit cannot be predicted. Vasodilators
are indicated in patients who refuse surgery or are not operative
candidates for any reason.
Vasodilators are also indicated for short-term therapy in patients
awaiting valve replacement to optimize their hemodynamics (reduce
filling pressures and increase cardiac output) and thus reduce
their operative risks. If LV systolic function is normal, they
can be given long-acting nifedipine. if they have abnormal LV
systolic function, they should be treated with digitalis and
ACE inhibitors; diuretics and hydralazine, with or without nitrates,
can be used if needed. Small doses of hydralazine (50 mg) are
without therapeutic effect in AR, and larger doses (approximately
100 mg) need to be given only twice daily; the twice-daily regimen
reduces the incidence of side effects. Hydralazine should be
started in small doses and gradually increased, depending on
patient tolerance of the drug.
Vasodilators are of considerable short-term benefit in patients
in functional classes III and IV or heart failure. All such
patients need digitalis, diuretics, and ACE inhibitors. In patients
in functional class IV with heart failure, vasodilators should
ideally be started after the institution of beside henmodynamic
monitoring-that is measuring of pulmonary artery wedge pressure
and cardiac output with the use of ballon flotation catheters.
Hemodynamic monitoring accurately identifies patients who need
the therapy, since clinical judgments can be wrong. It establishes
whether arterial dilators alone will suffice or whether additional
venodilators are needed. Finally, it provides information on
the optimum dosage of vasodilator therapy. After the initial
hemodynamic measurements are made, arterial dilators are given
in progressively increasing dosage until an optimum effect on
cardiac output has been obtained. If cardiac output does not
show any further increase but left atrial pressure is still
very high, additional venodilator therapy should be given. If
the patient is very ill or the hemodynamic abnormalities are
marked, intravenous therapy (e.g., sodium nitroprusside) is
the vasodilator of first choice. In this situation, intravenous
vasodilator therapy should be used only with bedside hemodynamic
monitoring. Inotropic agents, such as dobutamine, may be needed
to improve LV function and increase cardiac output. Low-dose
dopamine may be of value to increase urinary output.
Patients with severe chronic AR need valve
surgery. The correct timing of surgical therapy is now better
defined but is not fully clarified. Valve replacement should
be performed before irreversible LV dysfunction occurs. The
major problem, however, is identifying the precise point at
which LV dysfunction will occur. Here, two major difficulties
are encountered:
(1) patients may already have impaired LV systolic pump function
at rest when they firstpresent or at the time of the first symptom
and
(2) patients with severe symptoms may have normal LV systolic
pump function.
Patients may be in NYHA functional class III (symptoms with
less than ordinary activity), with a normal LV ejection fraction,
or they may be in functional class I (asymptomatic), with a
reduced LV ejection fraction. A reduced LV ejection fraction
demonstrated by two-dimensional echocardiography and/or radionuclide
ventriculography is the best noninvasive indicator of depressed
LV systolic function.
Decisions about surgery in AR should be based on the clinical
functional class and on the LV ejection fraction at rest (
Table 2 ) Patients with chronic severe AR who are symptomatic
(NYHA functional classes II to IV) need valve replacement. Although
there may be some disagreement about recommending valve replacement
to patients with normal ejection fraction who are in functional
class II, we currently would do so. The benefit from valve replacement
has been demonstrated even when the LV ejection fraction is
0.25 or less. As opposed to AS, in which there is no lower level
of ejection fraction that indicates inoperability, it is likely
that some patients with AR and a very low ejection fraction
become inoperable. This level has not been precisely defined
but may be about 0.15 or less. There is a need to individualize
the need for valve replacement in those with very severe LV
systolic dysfunction at rest, in those with very severe LV dilatation
(LV end-diastolic volume index approximately 300 mL/m2),’
and in those with a small regurgitant volume, with a ratio of
regurgitant volume to end-diastolic volume of 0.14 ( Table
2 ). Recent data indicate that patients with severe AR,
LV end-diastolic dimension on echocardiography of approximately
80 mm, and mild to moderate reduction of LV ejection fraction
(mean 0.43) can obtain benefit from valve replacement. Postoperatively,
they are symptomatically improved, LV ejection fraction increases,
and LV size is reduced; the 5-and 10-year survivals are 87 and
71 nercent. respectivelv.
Although.the issue is controversial in some
countries,we believe that patients who are in NYHA functional
class 1 (asymptomatc) and have a reduced ejection fraction at
rest should be offered aortic valve replacement. If the ejection
fraction is normal at rest, one should consider valve replacement
in NYHA functional class I patients if they have severe obstructive
CAD and/or need surgery for other valve disease ( Table
2 ). It is suggested that patients undergo an exercise test
during right heart catheterization if the left ventricle is
large (LV end-diastolic volume approximately 150 mL/m2, LV internal
dimension on M-mode echocardiography of approximately 70 mm
at end diastole and approximately 50 mm at end systole) and/or
the LV ejection fraction shows a new, persistent reduction to
0.54 to 0.60; if the patients have reduced exercise capacity
on treadmill testing; or if ambulatory ECG monitoring demonstrates
ventricular tachyarrhythmias. Valve replacement is recommended
if the pulmonary artery wedge pressure during exercise approximately
20 to 24 mmHg. Patients with associated significant CAD should
have coronary bypass surgery performed at the time of valvular
surgery .
Aortic valve replacement, with or without associated coronary
bypass surgery for obstructive CAD, can be performed at many
surgical centers with an operative mortality of 5 percent or
less. In those without associated CAD or reduced LV systolic
function, the operative mortality may be in the range of 1 to
2 percent. If aortic valve replacement is successful and uncomplicated,
LV volume and hypertrophy regress but do not return to normal;
the beneficial effects on LV size, volume, and mass continue
to be seen up to 5 years after surgery. Impaired LV systolic
pump function improves postoperatively in 50 percent or more
of patients; this improvement is more likely to occur if LV
dysfunction has been present preoperatively for 12 months or
less, and in this subgroup LV ejection fraction usually normalizes.
Even if LV systolic pump function does not improve, there is
a reduction in end-diastolic volume and hypertrophy; from a
cardiac point of view, this is advantageous to the patient.
The 5-year survival of patients undergoing aortic valve replacement
in severe AR is 85 percent (this figure includes operative and
late cardiac deaths). The 5-year survival of patients with LV
ejection fraction _0.45 is 87 percent, versus 54 percent in
patients with an ejection fraction <O.4S.1TM Late survival
after valve replacement for chronic severe AR is best predicted
by variables indicative of LV systolic pump function. Both the
operative mortality and late survival are dependent on cardiac
and LV function and associated noncardiac comorbid factors .
Indeed, in general, the major factors influencing
outcome in patients with valvular heart disease are: LV dysfunction
and its magnitude, duration of LV dysfunction, degree of LV
dilatation, greater NYHA functional class, older age, associated
CAD, and comorbid conditions.
New techniques of aortic valve repair are being developed and
evaluated, and early results are encouraging in selected subgroups.
It is possible that selected patients may eventually need to
have valve repair rather than valve replacement for AR.
The recommendations of the ACC/AHA Practice Guidelines are shown
in Table
3 Guidelines are not and should not be the Law. Application
of such guidelines to clinical practice should be based on the
following principles:
(1) classes I and III applies to all patients in these classes
unless there is a specific clinical circumstance not to do so;
(2) class II applies to patients in this class depending on
the clinical conditions of the patients and the skill and experience
at the individual medical center.
Rahimtoola,S.H.,Aortic Valve Disease,Hurst's
The Heart,10th Edition,Pages 1667-1692