Hypertension is a hemodynamic derangement.
The elevated blood pressure in systemic arterial hypertension
may be associated with an increased cardiac output or vascular
resistance (the hallmark of the disease).
Classification of the various
forms of hypertension based on causes are shown in table
2.
Reference:.Froblich,E.D.MD,Hurst's
The Heart.Pathophysiology of Systemic Arterial Hyper tension,pp1391-1401.
The major hemodynamic alteration in hypertension
is an increased vascular resistance, which is achieved through
an active increase in the state of tone of vascular smooth muscle
in both arterioles and the venules.
This state of vessel tone can be achieved whether
the myocyte is stimulated by enhanced adrenergic input (elevated
circulating levels) of humoral agents (e.g. catecholamines,
angiotensin II, vasopressin, serotonin), local vasoactive peptides
(e.g.angiotensin II, vasoactive intestinal polypeptide, endothelium),
or ions (e.g. calcium); by reduced amount of vasoconstrictors;
or by an increase in vasodilating agents (acetylcholine, adenosine,
prostaglandins), local vasoactive peptide (e.g. insulin, calcitonin
gene-related peptide), or ions (e.g. potassium, magnesium, Krebs
intermediate metabolites).
Whatever the myocyte stimulus, there is an increased
availability of calcium ions for the mechanical coupling that
permits the enhanced state of contractility of vascular smooth
muscle. Also, an increased wall to lumen diameter of the arterial
and arteriolar wall, serves to augment vascular responsiveness
to constrictive stimuli and perpetuates the hypertension.
The intravascular (plasma) volume contracts
in patients with essential hypertension and is associated with
a greater degree of interstitial fluid. If a the blood pressure
is lowered by a vasodilator drug, the capillary hydrostatic
and renal arterial perfusion pressure would diminish, causing
the interstitial fluid to migrate intravascularly to expand
the intravascular space and reducing the effectiveness of the
antihypertensive agent. But with the addition of a diuretic,
intravascular volume would again contract, thereby restoring
the anthypertensie effect.
Recently, the angiotensin converting enzyme
and the calcium channel inhibitor therapies have prevented the
expanded intravascular volume and pseudotolerance has been of
less concern.
Reference:.Froblich,E.D.MD,Hurst's
The Heart.Pathophysiology of Systemic Arterial Hyper tension,pp1391-1401.
Epidemiologic studies have demonstrated a high
direct correlation between dietary sodium intake of populations
and the prevalence of hypertension. The reduction in sodium
intake to levels below the current recommendation of 100 mmol
per day and the dietary approaches to stop hypertension diet
(DASH) both lower blood pressure substantially with greater
effects in combination than singly.
Reference:Sacks,F.,and
Others:Effects on blood pressure of reduced dietary sodium and
theDASH diet,N England J Med Vol.344,No.I, Jan.4,2001,pp3-9
;
Reference:.Froblich,E.D.MD,Hurst's The Heart.Pathophysiology
of Systemic Arterial Hyper tension,pp1391-1401.
Complications
of Hypertensive Disease
|
a. Left ventricular hypertrophy.
The left ventricle increases its mass and wall
thickness progressively as a result of the progressive overload
and increased left ventricular wall stress imposed by the increasing
arterial pressure and total peripheral resistance. Ultimately
a stable state is reached and subsequently diastolic dysfunction
occurs, associated with a fourth heart sound, atrial enlargement,
and reduced left ventricular distention.
Ultimately left ventricular systolic function
is impaired and cardiac failure occurs, if arterial pressure
and ventricular afterload are not reduced.
The best means of preventing of preventing morbidity and mortality
is to prevent left ventricular hypertrophy, using early and
continuous antihypertensive therapy.
b.
Myocardial ischemia and infarction.
Both of these complications may occur
due to increased LV pressure and LV chamber diameter leading
to increased oxygen demand in pure LV hypertensive heart disease.
Also, hypertension acclerates the onset of coronary atherosclerosis.
c. Aortic dissection
(to see the entire photographs of figures below click on the
tumbnails: 50, 51b, 51c, 51d, 51e, 51f, 51g, 51h, 51i, 51j,
51k).
Currently, the prevalence of this complication
has diminished due to the use of antihypertensive therapy (especially
beta blocking agents).
A recent study suggest that frequent follow-up
monitoring of patients having aortic intramural hematomas of
the ascending aorta (AIH) in the intensive care unit with CT,
transesophageal echocardiography, and MRI (figures above 51h,
51i, 51j, 51k) along with aggressive medical treatment of their
hypertension can be an option to allow timed surgical repair,
or prevent progression to dissection and rupture and improve
prognosis.
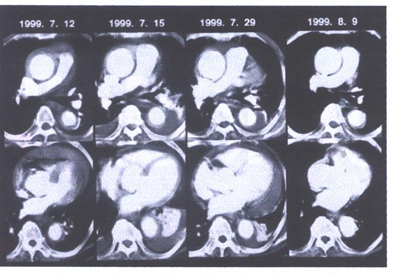
Fig.51i. Serial X-ray computed tomograms (CT)
in a patient with proximal aortic intramural hematoma (case
no. 18). Initial CT (July 12, 1999) showed characteristic crescentic
wall thickening in both the ascending and descending aorta with
a large amount of pericardial effusion. After emergent percutaneous
pericardiocentesis, medical treatment was chosen by the patient,
and CT (July 15, 1999) revealed development of pleural effusion.
The patient's condition stabilized rapidly, although the amount
of pleural effusion increased (July 29, 1999). One month after
the event, complete normalization of the aorta with resorption
of pleural effusion was observed (August 9, 1999).

Fig51j. One example of the development of typical
aortic dissection in a patient with proximal aortic intramural
hematnma (case no. 2). Initially, computed tomography showed
dramatic decrease of aortic wall thickening with progressive
enlargement of the lumen of the ascending aorta (October 31
and November 12). About two months after the event, she complained
of chest pain again and follow-up study revealed development
of typical aortic dissection
One predictive factor seems to be the size of
the ascending aorta at the first examination. It has been shown
that patients with an aortic diameter of less than 5cms. had
regression of the hematoma during medical therapy, whereas those
with a larger diameter had a tendency to progression to dissection
or rupture.
Also, the prognosis of very old patients is
acceptable under medical therapy because of severe atherosclerosis
apparently limiting the expansion of hemorrhage under blood
pressure control.
For patients with AIH, emergent surgery has
been the standard practice. But with close monitoring conditions
on an intensive unit, treatment strategies may be individualized.
Symptomatic patients and those with progression during follow-up
and a large ascending aorta should undergo emergent surgery.
But other patients whose condition can be stabilized with antihypertensive
therapy as well as very old patients may be treated medically
with good long-term results.
Reference:Song,J-K,MD,and others,Different
Clinical Features of Aortic Intramural Hematoma Versus Dissection
Involving the Ascending Aorta,JACC,Vol.37,No.6,2001,1603-1610.
Reference:Mohr-Kahaly,MD,Aortic Intramural
Hematoma:From Observation to Therapeutic Strategies,JACC,Vol.37,No.6,2001,1611-1613.
d.
Malignant and accelerated hypertension.
This form of hypertension is less common due to the widespread
use of antihypertension therapy. It represents a sudden accleration
in the vascular disease associated with essential hypertension
and if untreated results in over 97 per cent of involved patients
dying within one year.
It is associated with necrotizing arteriolitis
and severe arteriolar spasm,and reduced blood flow especially
to the kidneys, provoking a state of secondary hyperaldosteronism.
Vigorous antihypertensive treatment will reverse this positive
feedback mechanism.
e.
End stage renal disease and nephrosclerosis.
More frequently, essential hypertension is
associated with renal arteriolar thickening, fibrinoid deposition
in glomeruli, and proteinuria, which follow the development
of left ventricular hypertrophy.
f.
Parenchymal renal disease.
Hypertension is a frequent complication of most renal diseases,
whether glomerulonephritis, polycystic renal disease or others.
This type of hypertension should be considered in any case of
hypertension with anemia of undetermined cause, particularly
if that patient is black.
g. Strokes
Strokes have been dramatically reduced with
antihypertenaive therapy, whether hemorrhagic or thrombic, and
there has been at least a 50% reduction in fatal strokes.
Reference:.Froblich,E.D.MD,Hurst's
The Heart.Pathophysiology of Systemic Arterial Hyper tension,pp1391-1401.
How
Blood Pressure Is Measured
|
Blood Pressure is measured by means of a stethoscope
and an inflatable cuff (figure
122b) that compresses the arm until the brachial artery
is squeezed shut. Intially the artery walls will be closed and
no sounds will be heard through the stethoscope. As air is released
from the cuff a thump will be heard. This is the moment when
the systolic blood pressure-i.e. the first and higher of the
of the two numbers of a person's blood pressure-is recorded.
As the cuff pressure continues to drop below the level of the
systolic pressure, the artery will begin to open and close,
and a rhythmic thumping noise will be audible. When the sound
becomes muffled and faint, the diastolic pressure is recorded.
As the cuff pressure declines below the diastolic pressure in
the artery, the vessel remains open and the sounds disappear
completely (figure
122a).
The cuff size must match the patient's arm,
meaning a big arm requires a bigger cuff, and a smaller one
needs a smaller cuff.
Also, the patient should be sitting or lying
with the arm at the level of the heart while the reading is
obtained.
The patient should be relaxed. Finally caffeine,
nicotine and exercise should be avoided prior to taking the
blood pressure. If the reading is high, it should be repeated
after 2 to 3 minutes of relaxation and rest or later at another
appointment. Also, a 24 hour ambulatory monitor can be done
to check the pressure around the clock (figure
123e).
Reference:Harvard
Men's Health Watch,Feb.2001,pp.1-4
There is no single normal blood pressure; instead
blood pressure readings span a spectrum that ranges from ideal
at the low end to acceptable in the middle and abnormally high
at the top. Interpretations for adults 18 years of age and older
are in figure
123a.
Isolated
systolic hypertension
|
Isolated systolic hypertension with a normal
diastolic reading is the most common form of hypertension in
people 65 and older and its prevalence increases steadidly with
age (figure
123b,
123c). In a recent study of 15,693 people age 60 years old
or above and with systolic blood pressures of 160 or more and
diastolic pressures of 95 or less, without treatment each 10
mmHg rise in systolic blood pressure increased the risk of stroke
by 26%, with strokes accounting for much of the excess mortality.
Drug treatment reduced the risk of stroke by
30%,the risk of heart attacks by 23%, and the risk of death
by 13%.
Reference:Harvard
Men's Health Watch,Feb.2001,pp.1-4
High-Normal Blood Pressure
|
A recent study found that high-normal blood
pressure (systolic pressure of 130 to 139 mm Hg, diastolic pressure
of 85 to 89 mm Hg, or both) is associated with an increased
risk of cardiovascular disease, emphasizing the need to determine
whether lowering such pressures can reduce this risk.
Vasan,R.S. and others,Impact of high
normal blood pressure on the risk of cardiovascular disease,N
Engl J Med 2001;345:1291-7.,N
Engl
Treatment involves two elements, life style
modification and drug therapy. Diet should be low in sodium
and saturated fat but high in fruits, vegetables, whole grain,
and nonfat dairy products. Exercise, weight and stress control,
and limiting alcohol to no more than two drinks a day are important.
If these measures don't bring blood pressure
down or if there is organ damage or risk factors, then antihypertensive
drug therapy is necessary (figure 123d).
Most authorities suggest a diuretic first (table
6), then adding a beta blocker (table
7) particularly for older patients and those with isolated
systolic hypertension. Patients with diabetes or congestive
heart failure may get better results from angiotensin converting
enyzme (ACE) inhibitors (table
9), and with angina may benefit fron calcium channel blockers
(table
8).
The alpha1-adrenergic blocking agents (table
10) can be used as monotherary or in combination with other
existing progams. They are particularly effective in managing
hypertension associated with pheochromocytoma.
There are also alpha2-adrenoreceptor agonists
(aldomet, which is the preferred drug with hypertension and
ecclampsia; catapres, wytensin, tenex) prescribed as step 2
drugs due to side effects), neuroeffector adrenergic blocking
drugs (hylorel, ismelin, and reserpine, which is the least expensive,
effective, well tolerated) and direct vasodilators (hydralazine).
loniten reserved for multidrug resistant hypertension;
both usually prescribed with a beta-blocker to prevent tachycardia
and a diuretic to prevent edema).
Reference:Harvard
Men's Health Watch,Feb.2001,pp.1-4
Giffford,R.Jr.,Hurst's
The Heart,8th Edition,Treatment of Patients with Systemic Arterial
Hypretension.pp1427-1448
| Diagnostic
Evaluation of the Patient with Systemic Arterial Hypertension
|
Mild
to Moderate Hypertension
|
The clinician should inquire in the patient's
history about the existence of symptoms such as those listed
in table
3 , and perform the evaluation procedures and diagnostic
tests summarized in table
4.
One should look for clues to reversible causes
of the hypertension such as coarctation of the aorta including
diminished leg pulses, delay in the femoral pulse, reduced leg
blood pressure, a coarse systolic murmur at the left sternal
border or rib notching on the chest x-ray (figures
23a,
23b).
Acromegaly, thyroid diseases, Cushing's syndrome
and alcoholism should be suspected from the history and general
appearance of the patient.
In the evaluation a search for target organ damage and cardiovascular
risk factors should be made to include listening for bruits
over the carotid,renal and femoral arteries.
The EKG must be inspected for evidence of ischemia,
and the cholesterol and other tests recommended in table
4 should be performed.
It is important to examine for congestive heart failure by looking
for LVH, rales, ventricular gallop (heart sounds like a gallop),
distended neck veins, edema (swollen feet ankles, legs) amongst
other signs.
Severe,
Accelerated or Malignant Hypertension
|
Diagnostic criteria for malignant hypertension
include a diastolic blood pressure of 125mmHg or more, in conjunction
with target organ damage (retinal hemorrhages, papilla edema,
heart failure, encephalopathy, and renal insufficiency) and
physiologic abnormalities (impaired renal perfusion, elevated
plasma renin andaldosterone levels, increased sympathetic tone).
Renal arteriography may be necessary to diagnose
renal artery stenosis.Also,a plasma catecholamine level is indicated
as well to rule out pheochromcytoma.
Athlete
with Hypertension
|
Marfan's sydrome with aortic regurgitation
and hypertrophic cardiomyopathy (figures 39,
39b,
39f)
must be considered.
Echocardiography should be considered in athletes
with abnormal EKG's suggesting LVH with abnormal ST- and T-
wave changes (echocardiographic septal or posterior LV wall
thickness of 13mm or more are uncommon in atheletes with physiologic
LVH).
| DIAGNOSIS
OF TARGET ORGAN DAMAGE |
Advanced retinopathy is associated with a poor
prognosis.
Hypertensive
Cardiovascular Disease
Two major forms of heart disease occur in patients with hypertension:
coronary heart disease (discussed elsewhere on this website)
and hypertensive heart disease. The criteria for hypertensive
heart disease include the presence of hypertension plus LVH
when other causes are excluded.These patients may be susceptible
to myocardial ischemia without evidence of coronary disease.
The EKG is one of the tests used to detect LVH
(table
5).
EKG evidence of left atrial abnormality often
precedes the LV abnormality:
terminal negative atrial forces in V1 above 0.04mm-s, bipeak
interval > 0.04s in deeply notched P waves in any lead,ratio
of P wave duration to PR interval exceeding 1.6 in leadII,and
P wave above 0.3mv height or above 0.12 duration in leadII.
Echocardiographic evidence of LVH (assessing
IVS thickness,LV posterior wall and free wall thickness) occurs
in 30-40% of hypertensive patients whose EKG and chest appear
normal. Thus, the echocardiogram is an early and sensitive indicator
of LVH in patients with hypertension.
Hypertensive
Cerebrovascular Disease
Cerebrovascular
Accidents
|
Hypertension is the most important risk factor
for the development of hemorrhagic or atheroembolic stroke.
Microhemorrhage or occlusion of small vessels can result in
small areas of infarction (lacunar infarcts), which are associated
with neurologic deficits that clear over days to weeks. Multiple
lacunas can lead to to multi-infarct dementia. The differentiation
between a transient ischemic attack (TIA) and a small lacunar
infarct may be difficult but MRI may be able diagnose these
lacunas.
Evanescent neurologic symptoms or findings in
conjunction with a carotid artery bruit justify carotid duplex
Doppler scan and/or angiography in an operable patient.
Hypertensive
Encephalopathy
|
Hypertensive encephalopahy is characterized
by acute to subacute changes in neurologic status that occur
as a result of elevated arterial pressure (especially malignant
hypertension) and are reversed by lowering of the blood pressure
with effective antihypertensive therapy within 12 to 72 hours.
The CT scan and MRI can help diagnose focal areas of intracerebral
hemorrhage or infarction.
Hypertensive Nephrosclerosis
Benign Nephrosclerosis
Malignant Nephrosclerosis
| DIAGNOSIS
OF SECONDARY CAUSES OF HYPERTENSION |
Renovascular
Hypertension Prevalence
|
Renal artery stenosis is the most common curable
of hypertension, but probably occurs in 3% or less of hypertensive
patients. Below the age of 40, renovascular hyprtension is more
frequent in women than men and is less common in the black patients
with hyprtension.
Abdomiminal bruits and severe hypertensive retinopathy
are clues to renovascular disease.
Pathological Types of Renal Artery Stenosis
Fibrous dysplasia and atherosclerosis of the
renal arteries account for almost all cases of renovascular
hypertension.
1. Fibrous Dysplasia
With fibrous dysplasia , hypertension generallly
presents before age 35, most often in women. It is usually unilateral
when initially diagnosed. In 60% of cases there is an upper
abdominal bruit (figure
140 ).
Reference:Safian.R.and
others.RENAL ARTERY STENOSIS,N.Engl.J.Med.Vol.344,No.6,Feb.8,2001.pp431-442
).
2. Atherosclerotic Renovascular Disease
It accounts for two-thirds or more of the patients
with renovascular hypertension, occurring predominantly in men
over 45 years (figure
140 ). At least two-thirds have bilateral lesions (Progressive
atherosclerosis, renal artery stenosis and ischemic nephropathy,
figure
141)
Reference:Safian.R.and
others.RENAL ARTERY STENOSIS,N.Engl.J.Med.Vol.344,No.6,Feb.8,2001.pp431-442
).
Diagnostic Tests are not indicated in patients
with advanced renal failure and bilateral small kidneys.
Reference:Hall,W.D.,AND
OTHERS, Diagnostic Evaluation of the Patient with Systemic Arterial
Hypertension,HURST'S 8TH Edition,The Heart,pp.1403-1425.
(Figure126,
Reference:Safian.R.and others.RENAL ARTERY STENOSIS,N.Engl.J.Med.Vol.344,No.6,Feb.8,2001.pp431-4420
)
Digital subtraction Angiography or Aortography
When the clinical suspicion is high, it is usually
more expedient to proceed directly to arterial DSA or arterigraphy.
Reference:Safian.R.and
others.RENAL ARTERY STENOSIS,N.Engl.J.Med.Vol.344,No.6,Feb.8,2001.pp431-442
).
Reference:Hall,W.D.,AND OTHERS, Diagnostic Evaluation of the
Patient with Systemic Arterial Hypertension,HURST'S 8TH Edition,The
Heart,pp.1403-1425.
Renal vein Renin Ratio (table2a,
Noninvasive Assessment of Renal-Artey Stenosis)
Once the presence of renal arterial disease has been
established, the functional significance of the stenosis can
be evaluated to help determine if the renal artery lesion is
the cause of the hypertension, by measuring the renal vein renin
ratio.A renal vein ratio of 1.5 or greater favoring the stenotic
side is indicative of a functional significant renal artery
lesion.
The renal vein renin ratio is frequently not
reliable for predicting surgical response in patients with bilateral
renovascular disease (figure
142 )
Reference:Safian.R.and
others.RENAL ARTERY STENOSIS,N.Engl.J.Med.Vol.344,No.6,Feb.8,2001.pp431-442
.
Reference:Hall,W.D.,AND OTHERS, Diagnostic Evaluation of the
Patient with Systemic Arterial Hypertension,HURST'S 8TH Edition,The
Heart,pp.1403-1425.
Captopril Renography
Isotope renography detects the acute reductions
of glomerular filtration rate(GFR) following the administration
of captopril to patients with functionally significant renal
artery stenosis and is often an effective screening procedure
for renovascular hypertension. Isotope renography using 99m
Tc-DPTA (reflecting largely glomerular filtration rate) is performed
immediately before and 60 to 90 min. after the administration
of a single 2.5-mg dose of captopril. Following converting enzyme
inhibition,both the uptake and excretion of DPTA on the stenotic
side are usually decreased from baseline in patients with unilateral
renal arterial disease, whereas no consistent decrease is observed
in the contralateral uninvolved kidney (figure 124a).
Reference:Goto,A.
and others,Captopril-Augmented Renal Scan,N.Engi.J.Med.Vol.344,No.6,Feb.8,2001,p430).
This acute reduction in filtration rate that
occurs in the stenotic kidney following converting enzyme inhibition
may be due to interruption of angiotensin II-mediated vasoconstriction
of the postglomerular efferernt arteriole.
Reference:Hall,W.D.,AND
OTHERS, Diagnostic Evaluation of the Patient with Systemic Arterial
Hypertension,HURST'S 8TH Edition,The Heart,pp.1403-1425.
Atherosclerotic renal-artery stenosis is a common
sign of generalized atherosclerosis (figure
142 ) and is frequently associated with hypertension and
excretory dysfunction (figure
141). But the association of renal-artery stenosis with
hypertension or renal insufficiency does not establish causation,
and although the methods for the diagnosis and treatment of
renal insufficiency have improved, the use of invasive diagnostic
techniques and treatment early in the course of the disease
still has no proven benefit.
Further, there seems to be a shift away from
identifying patients with renovascular hyprtension, because
of the known benefits of medical therapy and lack of sustained
cure after percutaneous or surgical revascularization, and a
shift toward identifying patients with renal artery stenosis
who are at risk for excretory dysfunction.
Because of this shift, medical therapy and modification
of risk factors to limit atherosclerosis are essential in all
patients, regardless of whether they have undergone revascularization.
In patients with atherosclerotic renal-artery
stenosis who are at risk for excretory dysfunction, percutaneous
and surgical techniques may improve or stabilize renal function.
The long term results are better in patients who have better
renal function at base line, suggesting that deferring revascularization
until renal function deteriorates may not be the best approach.
Reference:Safian.R.and
others.RENAL ARTERY STENOSIS,N.Engl.J.Med.Vol.344,No.6,Feb.8,2001.pp431-442
Doppler ultrasonography can determine the resistance
to flow in the segmental arteries of both kidneys ( high level
of resistance indicated by resistance-index values of at least
80) , the values for which can be used to predict patients whose
renal function or blood pressure will improve after the correction
of renal -artery stenosis. A renal resistance index value of
at least 80 reliably identifies patients with renal-artery stenosis
in whom angioplasty or surgery will not improve renal function,
blood pressure, or kidney survival.
Reference:Radermacher,J.
and Others, Use of Doppler Ultrasonography
To Predict The Outcome Ofe used to predict patients
whose renal function or blood pressure will improve after the
correction of renal-artery stenosis. A renal resistance index
value of at least 80 reliably identifies patients with renal-artery
stenosis in whom angioplasty or surgery will not improve renal
function, blood pressure, or kidney survival.
Reference:Radermacher,J.
and Others, Use of Doppler Ultrasonography To Predict The Outcome
Of Therapy For Renal-Artery Stenosis,N.Engl. J.Med .2001;344:410-7
TREATMENT
OF PRIMARY PULMONARY
HYPERTENSION - THE NEXT GENERATION
PRIMARY pulmonary hypertension predominantly
affects women, frequently in the prime of life, and usually
leads to death from right ventricular failure within a few years
after diagnosis. It is a vascular disease but is oddly confined
to the small pulmonary arterioles, where intimal fibrosis and
medial hypertrophy lead sequentially to vascular obstruction,
elevated pulmonary vascular resistance, pulmonary hypertension,
and right ventricular overload. Coagulation at the endothelial
surface contributes to obstruction, and thromboembolism may
occur as a secondary event. The right ventricle compensates
through hypertrophy, and although it can sustain function at
high pressures for months to years, decompensation is ultimately
manifested in reduced cardiac output and the development of
peripheral edema. Many conditions and diseases lead to similar
pulmonary vascular lesions and clinical outcomes, including
the scleroderma spectrum of diseases, human immunodeficiency
virus infection, liver disease, and the use of certain anorectic
drugs.These illnesses, along with primary pulmonary hypertension,
are now classified as types of pulmonary arterial hypertension.
Primary pulmonary hypertension first came under coordinated
scientific scrutiny when the National Institutes of Health created
the national Primary Pulmonary Hypertension Patient Registry
in 1982, at a time when there was increasing optimism about
a role for vasodilator therapy. Although there had been multiple
previous reports of benefit from beta-agonists, alpha-blockers,
and hydralazine, these responses were usually not sustained,
and the relevant studies were not appropriately powered to detect
true effects. The discovery that calcium-channel blockers could
cause a sustained reduction in pulmonary vascular resistance
in about 20 to 25 percent of previously untreated patients led
to aggressive approaches to short-term vasodilator testing and
long-term vasodilator therapy. Although not every patient with
acute vasodilatation has a durable response to therapy, this
feature carries a favorable prognosis, and many such patients
are treated with calcium-channel blockers alone. It has not
been proved that vasoconstriction is a pathogenetic mechanism
of primary pulmonary hypertension, but this possibility seems
logical and deserves continued study.
What can be done for the 75 percent of patients who do not have
a response to short-term vasodilator therapy? The discovery
that intravenous epoprostenol (prostacyclin) improved functional
capacity, not only in patients with a response to calcium-channel
blockers but also in those without a response, was followed
by evidence that it also improves survival among both types
of patients.This finding has led to widespread use of continuous
intravenous epoprostenol therapy in all patients without a response
to calcium-channel blockers and in most patients with New York
Heart Association class IV heart failure. Beyond the activity
of epoprostenol as a potent vasodilator, its mechanisms of benefit
are unclear, but they may indude a positive inotropic effect,
a small degree of systemic vasodilatation, and antiplatelet
effects, which theoretically could reverse vascular damage.
Epoprostenol therapy by continuous infusion through a central
catheter is expensive - about $60,000 per year - as well as
technically demanding, and it has undesirable side effects.
It is widely recognized that simpler effective therapies are
needed. Prostacyclin analogues given by continuous subcutaneous
infusion, orally, or by intermittent aerosol are under development
as alternatives to the intravenous route. Subcutaneous treprostinil
was recently approved by the Food and Drug Administration for
further clinical trials. The prostacyclins act through an increase
in the level of the second messenger, intracellular cyclic AMP
(cAMP). Other vasodilators, including inhaled nitric oxide and
oral sildenafil, act by means of cyclic guanosine monophosphate
(cGMP). Sildenafil increases the cGMP level by inhibiting phosphodiesterase
type 5, an enzyme that hydrolyzes cGMP. Clinical studies are
needed to test for potential additive effects of simultaneous
increases in cGMP and cAMP by combining the two classes of drugs.
Safe generation of nitric oxide in vivo might be attained with
the use of oral arginine or citrulline, substrates for the generation
of nitric oxide, with resultant cGMP levels sustained by concomitant
oral sildenafil.
Endothelin-1 is a potent endogenous peptide mediator that has
a role in pulmonary arterial hypertension. It is unclear whether
it has a primary pathogenetic role or whether it is a secondary
mediator that perpetuates disease. Plasma endothelin levels
are increased in patients with primary pulmonary hypertension,
and endothelin is released in increased amounts in the blood
traversing the lung. Endothelin is released by endotheial cells
as big endothelin, which is cleaved to pro-endothelin, which,
in turn, is converted to endothelin-1 (in systemic and lung
vessels) or endothelin-2 (in kidney and gut). Endothelin-1 acts
on two receptors - endothein-A receptors and endothein-B receptors.
Activation of endothelin-B receptors causes the production of
nitric oxide and vasodilatation, and activation of endothelin-A
receptors results in vasoconstriction and smooth-muscle growth.
The ideal endothein-receptor antagonist is likely to be specific
for endothelin-A.
A study using bosentan, a nonspecific endothelin receptor antagonist,
to treat pulmonary hypertension is reported in this issue of
the Journal. Bosentan had small but measurable beneficial effects
in a double-blind, placebo-controlled trial involving 213 patients.
The duration of this trial was 16 weeks, which is not sufficient
to test for a difference in mortality, but its results suggest
that endothelin-receptor blockade has a therapeutic role in
some patients with pulmonary arterial hypertension. The effect
of bosentan appeared to be limited in most patients, and there
was an unacceptable incidence of abnormal hepatic function at
the higher dose. Because short-term vasodilator testing was
not performed as part of the study, it is not known whether
the patients with the best response to the drug were the same
patients who might have had a response to other vasodilators.
One cannot conclude from this study that bosentan should be
the primary drug for the treatment of primary pulmonary hypertension
or of other causes of pulmonary arterial hypertension. Follow-up
studies are needed to determine the durability of the effect,
whether there are differences in survival, what types of complications
occur, and whether subgroups of patients have different responses
to the drug. It would be useful to measure endothelin levels
and to determine whether there are correlations between these
levels and clinical effects. Studies should be designed to test
whether combining endothelin-receptor antagonists with either
inhibitors of phosphodiesterase type 5 or inducers of cAMP results
in greater functional improvement than does either class of
drug alone.
No current therapies appear to affect the pathogenesis of pulmonary
vascular obstructive disease directly. In rare cases, patients
receiving epoprostenol have had such dramatic responses that
the dose has been reduced, and cessation of drug therapy has
been attempted in a few patients, although the outcomes have
not been published. The recent discovery that the transforming
growth factor beta(TGF-beta) superfamily of receptors is involved
in the pathogenesis of pulmonary hypertension should lead over
the course of the next several years to specific therapies aimed
at the origin of the disease. The evidence suggesting the involvement
of TGF-beta receptors is compelling. About half of studied patients
with familial primary pulmonary hypertension have mutations
in exons of the bone morphogenetic protein receptor II gene
(BMPR2), and the majority of others have genetic linkage to
areas of chromosome 2 near BMPR2, perhaps in a promoter or upstream
regulator or perhaps in intronic DNA. In addition, about 25
percent of patients with sporadic primary pulmonary hypertension
have been found to have mutations in BMPR2. Mutations in the
gene for activin-receptor-like kinase 1 (ALK1), another receptor
in the TGF-beta family, are responsible for pulmonary hypertension
in at least some patients with hereditary hemorrhagic telangiectasia.
Clusters of endotheial cells carrying somatic TGF-beta 2-receptor
mutations are found in plexiform lesions in the pulmonary arterioles
of patients with sporadic primary pulmonary hypertension. Studies
of these receptor abnormalities in transfected cells, cell cultures
from patients' tissues, and transgenic mice are under way, and
insights into the relevant mechanisms will certainly emerge
during the next several years. Other promising areas of research
are potassium-channel function and drugs that interrupt the
cycle of growth and repair in diseased pulmonary vessels.
Therapy for primary pulmonary hypertension has progressed from
calcium-channel blockers to prostacydin and now includes adjunctive
therapy with bosentan and, in some patients, sildenafil. Combination
therapies should be tested in the next generation of studies.
It now seems conceivable that the continuous intravenous administration
of epoprostenol through a central catheter will soon be history.
A better understanding of pathogenesis is at hand because the
genes associated with many cases of primary pulmonary hypertension
have been identified, but the development of therapies based
on this knowledge awaits further insights.
JOHN H. NEWMAN, M.D.
Vanderbilt University School of Medicine
Nashville, TN 37232
Newman,J.H.,N Engl Med,Vol.346,No.12,March21,2002
Pp.933-935.